Research article / Open Access
DOI: 10.31488/bjcr.184
A Comparative Study of Symptom Prevalence between Adults and Elderly Patients with Advanced Cancer Diagnosis Under Palliative Care: A Single Institution Experience
Hodan Abdullah*1, Ayman Allam1, Shaikhah Al keldi1, Zeinab Idris1,Azza Hassan1,3, Kalpana Singh2, Badriya Al Lenjawi2
1. National Center for Cancer Care and Research, Hamad Medical Corporation, Doha, Qatar
2. Nursing Research Department, Hamad Medical Corporation, Doha, Qatar
3. Cancer Management & Research, Medical Research Institute, Alexandria University, Alexandria, Egypt
*Corresponding author:Hodan Abdullah, National Center for Cancer Care and Research, Hamad Medical Corporation, Doha, Qatar
Abstract
Introduction: Analysis of the most common prevalent symptoms among patients with advanced cancer diagnosis is needed in order to reach the most appropriate interventions leading to improved quality of life of these patients. Aim: To report on the overall symptom prevalence among patients with advanced cancer diagnosis under palliative care and to analyze the difference of symptom prevalence between elderly (≥ 65 years) and adult (<65 years) patients. The study also will compare PPS score between the two groups as well as the most common cancer types in both groups.Methods: A retrospective cohort study of 400 patients with advanced cancer admitted under palliative care between 1st January 2017 to December 31st, 2021. Data were retrieved from electronic medical records. Results: Anorexia (91%), fatigue (98%), drowsiness (84%) and pain (83%) were the highest four prevalent symptoms for the whole group, followed by depression (76%) and anxiety (72%). Adult patients had significant higher pain (80% versus 76%), depression (83% versus 68%) and anxiety (77% versus 65%), compared to elderly (≥ 65 years) patients. On multivariate analysis, pain only was significantly higher in adult patients (p=0.021). The reported percentage of symptom prevalence for the whole group is higher than that in the literature, indicating late referral to palliative care.
Conclusion: There is a high percentage of symptom prevalence among patients in this current study and a short median overall survival that indicates late referral to palliative care. Adult patients had significantly higher pain, depression, and anxiety compared to elderly patients. An earlier integration of palliative care is needed in the overall management of patients’ symptoms.
Key words:symptoms, advanced cancer, prevalence, elderly, young adult, palliative care
Introduction
A comprehensive assessment of patients with advanced progressive cancer diagnosis should include physical, psychological, social, and spiritual aspects.The analysis of the most prevalent symptoms encounteredin this group of patients, especially those under palliative care, helps in addressing the needed interventions to improve common symptoms. Hence, improving the quality of life of those patients and their families or caregivers.
Most of the literature reported that pain and fatigue are the most common symptoms with the highest prevalence (70%-80%) in patients with advanced progressive cancer transferred under palliative care; this is usually followed by anorexia and weight loss, dyspnea, and nausea and vomiting (ranging from 40%-50%). Anxiety and depression are usually on the lower range (between 15%-20%); however, their prevalence increases considerably at the end of life and may reach up to 60% [1].
Research focusing on symptom prevalence in elderly (≥ 65 years) patients with advanced progressive cancer is scarce. Despite that the majority of older people are aging well, the incidence of frail older persons with advanced symptomatic progressive cancer is increasing. Whether we can extrapolate the results of symptom prevalence in younger patients to apply it to the older population with advanced cancer is questionable.
The Edmonton Symptom Assessment Scale (ESAS) is one of the most reliable, reproducible, and validated tools to analyze the most common symptoms in patients with advanced progressive cancer which is used in palliative care [2,3].The ESAS was first developed in 1991 by Bruera and colleagues for daily auditing of symptoms’ severity for patients on palliative care wards. The initial version consisted of eight items: pain, activity, nausea, depression, anxiety, drowsiness, appetite, and sensation of well-being. A ninth item was added to document ‘‘a less frequent symptom that might be important for a given patient’’ [3].
Later, ESAS has been validated by multiple research groups, and several studies have examined patients’ perceptions of ESAS and reported a need for improvement. These findings led to the proposal of a revised ESAS (ESAS-r) that consists of nine core symptoms: pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, feeling of well-being, and shortness of breath. The severity of each symptom is graded from 0 to 10. The ESAS can be completed by patients, relatives, or nurses [3]. This single-page screening tool has been praised for its brevity and ease of use, and it is frequently described as a practical, reliable, and valid tool [4].
Many prognostication tools have been used in palliative care to accurately predict prognosis in patients with advanced progressive cancer and overall survival time. This helped in reaching timely clinical, ethical, and operational decisions regarding the care plan for those patients [5]. One of these tools is the Palliative Performance Scale (PPS), which is used at the National Center of Cancer Care and Research (NCCCR) in Qatar. It has been reported as a sensitive, reliable, and reproducible prognostication tool that has been used to estimate prognosis in patients with advanced progressive cancer diagnosis who have been transferred under palliative care [6]. It consists of 11 categories with 10% increments from 0% (dead) to 100% (completely normal) depending on variable factors such as ambulation, oral intake, consciousness level, self-care, activity, and evidence of disease [5,6].
The primary aim of the present study is to compare symptom prevalence between adults (<65 years) and elderly (≥ 65 years) patients with advanced cancer diagnosis under palliative care. The study also will compare PPS score between the two groups as well as the most common cancer types in both groups.
Methodology
Study design
This is a retrospective cohort study. Data were retrieved from the electronic medical record from January 1st, 2017 to December 31st, 2021 for all advanced cancer patients who were transferred from active anticancer treatment to palliative care in the NCCCR in Qatar. Demographic data included were age, gender, and the primary site of cancer. The symptoms were assessed through the Edmonton Symptom Assessment System (ESAS) tool at the first day of acceptance under the palliative care program.
Population
This study included all adult patients (>14 years of age) with the diagnosis of advanced and progressive cancer who were admitted to the NCCCR and accepted under the palliative care program. The study excluded patients who had no initial ESAS assessment documented in the EMR when transferred under the palliative care program.
Statistical analysis
In the univariate analysis, associations between patient variables and younger (<65 years) and elderly (≥ 65 years) patients were examined using descriptive statistics and the chi-square test (gender, type of cancer, initial PPS, and symptoms). A p-value less than 0.05 was considered statistically significant. Patient variables which were identified as significantly associated with age (younger vs. elderly) in the univariate analysis were further analyzed with multivariate logistic regression to adjust for potential confounding variables, with associations expressed as odds ratios (ORs) with 95% confidence intervals (CIs). All tests were two-sided, and all statistical analysis was done using STATA 17.0.
Results
There is a total of 400 patients included in this study. There were 230 (58%) patients ˂ 65 years of age, compared to 170 (42%) patients ≥ 65 years of age. The median age of patients < 65 years was 54 years with a range of (15 years to 64 years) and the median age of patients ≥ 65 years was 72 years with a range of (65 years to 94 years)
Table 1 shows the characteristics of patients in both groups. There was no difference between male and female ratios in the two groups. GIT tumors were the most common cancer type in both age groups, with incidence rates of 19% and 22% in patients ˂ 65 years and ≥ 65 years, respectively.
Table 1.Patient characteristics according to age group
| Factor | Level | < 65yrs | >=65 yrs | p-value |
|---|---|---|---|---|
| N | 230 | 170 | ||
| Gender | Male | 110 (47.8%) | 81 (47.6%) | 0.97 |
| female | 120 (52.2%) | 89 (52.4%) | ||
| Type of cancer | Brain | 10 (4.3%) | 7 (4.1%) | 0.45 |
| Breast | 38 (16.5%) | 18 (10.6%) | ||
| GI | 43 (18.7%) | 37 (21.8%) | ||
| Gynecology | 28 (12.2%) | 23 (13.5%) | ||
| Hematology | 6 (2.6%) | 7 (4.1%) | ||
| Hepatobiliary | 43 (18.7%) | 28 (16.5%) | ||
| Lung | 15 (6.5%) | 19 (11.2%) | ||
| Other | 47 (20.4%) | 31 (18.2%) | ||
| Initial PPS score (in the day of acceptance) | 10% | 4 (1.7%) | 8 (4.7%) | 0.32 |
| 20% | 9 (3.9%) | 8 (4.7%) | ||
| 30% | 110 (47.8%) | 90 (52.9%) | ||
| 40% | 58 (25.2%) | 38 (22.4%) | ||
| 50% | 33 (14.3%) | 19 (11.2%) | ||
| 60% | 4 (1.7%) | 1 (0.6%) | ||
| 70% | 12 (5.2%) | 5 (2.9%) | ||
| 80% | 0 (0.0%) | 1 (0.6%) |
Hepatobiliary tumors were the second most prevalent cancer type in both age categories, with an incidence of 19% and 17% in patients 65 years and 65 years, respectively. Primary lung cancer was significantly more prevalent in elderly patients (11%) than in adult patients (6.5%), but this difference was not statistically significant.
The only difference in initial PPS score between the two age groups was a higher percentage of PPS score of 10% in the elderly group (5%) vs. (2%) in the adult group and a higher percentage of PPS score of 70% in the adult group versus the elderly group (5% versus 3%). As for the remaining PPS score levels, there was no difference between the two age groups.
In terms of symptom prevalence for the entire group (400 patients), anorexia (91%), fatigue (98%), drowsiness (84%), and pain (83%) were the highest four prevalent symptoms; followed by depression (76%), anxiety (72%), and to a lesser extent dyspnea (67%) and nausea (61%), as shown in table 2.
The presence of advanced, progressive cancer negatively impacted the health of nearly all patients (97 to 99 percent). When compared to elderly patients (≥ 65 years) as regards symptom prevalence, adult patients (˂ 65 years) had significantly higher pain (89% versus 76%; p=<0.001), depression (83% versus 68%) p=<0.001), and anxiety (77% versus 65%, p=0.005). The same results were found as regards anorexia prevalence (94% versus 86%) for adults versus elderly patients respectively (p=0.004). The prevalence of fatigue, nausea, and dyspnea was similar in both age groups (Table 2).
Table 2.Symptom prevalence in younger and elderly patients
| Factor | Level | Total | < 65 yrs | ≥65yrs | p-value |
|---|---|---|---|---|---|
| N | 400 | 230 | 170 | ||
| Pain | Absent | 67 (16.8%) | 26 (11.3%) | 41 (24.1%) | < 0.001 |
| Present | 333 (83.3%) | 204 (88.7%) | 129 (75.9%) | ||
| Tiredness | Absent | 8 (2.0%) | 4 (1.7%) | 4 (2.4%) | 0.66 |
| Present | 392 (98.0%) | 226 (98.3%) | 166 (97.6%) | ||
| Drowsiness | Absent | 65 (16.3%) | 34 (14.8%) | 31 (18.2%) | 0.35 |
| Present | 335 (83.8%) | 196 (85.2%) | 139 (81.8%) | ||
| Nausea | Absent | 156 (39.0%) | 81 (35.2%) | 75 (44.1%) | 0.071 |
| Present | 244 (61.0%) | 149 (64.8%) | 95 (55.9%) | ||
| Lack of Appetite | Absent | 37 (9.3%) | 13 (5.7%) | 24 (14.1%) | 0.004 |
| Present | 363 (90.8%) | 217 (94.3%) | 146 (85.9%) | ||
| Shortness of Breath | Absent | 131 (32.8%) | 68 (29.6%) | 63 (37.1%) | 0.11 |
| Present | 269 (67.3%) | 162 (70.4%) | 107 (62.9%) | ||
| Depression | Absent | 94 (23.5%) | 40 (17.4%) | 54 (31.8%) | < 0.001 |
| Present | 306 (76.5%) | 190 (82.6%) | 116 (68.2%) | ||
| Anxiety | Absent | 112 (28.0%) | 52 (22.6%) | 60 (35.3%) | 0.005 |
| Present | 288 (72.0%) | 178 (77.4%) | 110 (64.7%) | ||
| Wellbeing | Absent | 7 (1.8%) | 2 (0.9%) | 5 (2.9%) | 0.12 |
| Present | 393 (98.3%) | 228 (99.1%) | 165 (97.1%) |
Patient symptoms (pain, appetite, depression, anxiety, and anorexia) were identified as having a significantly higher prevalence in patients < 65 years' age compared to patients ≥ 65 years’ age in univariate analysis. In multivariate logistic regression analysis, only the absence of pain remained significantly associated with older age (OR 1.95, 95% CI: 1.1,3.45, p = 0.021 (Table 3).
Table 3.Multivariate Logistic Regression Analysis of patients in comparison to patients as regards symptom prevalence < 65yrs ≥ 65yrs.
| odds(95% CI) | P value | ||
|---|---|---|---|
| Pain | Present | Ref | |
| Absent | 1.95 (1.1,3.45) | 0.021 | |
| Lack of Appetite | Present | Ref | |
| Absent | 1.67 (0.77,3.63) | 0.195 | |
| Depression | Present | Ref | |
| Absent | 1.56 (0.86,2.82) | 0.144 | |
| Anxiety | Present | Ref | |
| Absent | 1.24 (0.72,2.14) | 0.437 |
The median survival for the whole group was 17 days (with a range of 7-40 days). The median survival for elderly patients was higher than that of younger adults (20 days versus 16 days, p=0.078); however, this difference was not statistically significant (Figure 1).
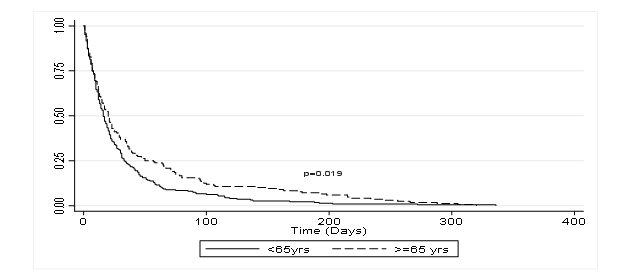
Figure 1:Overall survival between young and elderly patients
Discussion
In oncology practices, elderly patients (≥ 65 years of age) constitute a significant proportion of the patient population and require special consideration for symptom assessment and management. Research concerning a comparative analysis of symptom prevalence in elderly (≥ 65 years) versus younger adults (<65 years) is scarce. The present study also reported on the prevalence of symptoms for the entire cohort of patients with advanced cancer transferred under palliative care to NCCCR, the only cancer care facility in Qatar. Fatigue, anorexia, pain, lethargy, and depression were the most prevalent symptoms among the entire population, followed by anxiety, dyspnea, and nausea. This was similar to studies conducted by Omran et al. [7] and Dhingra et al. [8], but the symptoms were ranked differently, with fatigue and pain being the two most prevalent. This study's finding that fatigue was more prevalent than pain is supported by the majority of the literature on patients transferred to palliative care [9,10]. In addition, Dhingra et al. [8] study of the prevalence of symptoms in a large group of patients revealed that fatigue and pain were the most common, with fatigue being deemed the most distressing symptom.
It has also been noticed in the present study that there is a much higher prevalence of anxiety and depression in comparison to published literature, where anxiety and depression were less reported by patients [11,12]. This higher percentage in the current study could be attributed to two main factors: the late referral to palliative care compared to referral practice in Europe and North America’s health care systems as well as a higher percentage of expatriates in Qatar who come to the country without social support, are bachelor, and at a younger age, which predisposing them to a higher percentage of anxiety and depression, especially when diagnosed with advanced cancer.
One of the primary aims of this research was to compare the prevalence of symptoms between two groups, adults (< 65 years) and elderly (≥ 65 years) patients with a diagnosis of advanced progressive cancer. Data of this study showed a similar prevalence as regards fatigue, drowsiness, nausea, dyspnea between the two age groups. However, pain, depression, anxiety, and anorexia were more prevalent in the younger adult group (<65 years) than in the elderly patient group (≥65 years). This significantly higher prevalence of anxiety and depression in the younger age group (<65 years) confirms that this age group consists primarily of expatriates who come to Qatar to work, mostly without family or social support. It also reflects the greater psychosocial burden, which was introduced by Cicely Saunders in the 1960s as part of the total pain concept [13].
In accordance with previous studies Hagarty et al. and Barbera et al. [14,15] the prevalence of discomfort was higher in the younger age group (<65 years). In Hagarty and colleagues' (2020)[14] retrospective population-level cohort study involving more than 20,000 patients, the prevalence of pain was higher among younger patients (63%) than among elderly patients (44%). The current study's finding of a lower prevalence of symptoms among elderly patients compared to younger patients was consistent with findings of Cataldo et al. [16] study. They used the Memorial Symptom Assessment Scale to evaluate the occurrence, severity, frequency, and distress of 32 symptoms. The incidence, severity, and distress of symptoms were considerably lower in elderly patients (≥60 years) than in younger patients (<60 years). A second prospective observational study on cancer patients undergoing radiotherapy revealed that the total symptom burden worsened during radiotherapy for both elderly and younger patients, negatively impacting their quality of life. Younger patients reported substantially worse pain, nausea, and insomnia after completing radiotherapy than older patients [17].
In 2012, Kirkovaet al. [18]investigated 38 symptoms in 1000 consecutive patients with advanced cancer diagnosis, and found a higher frequency of eight symptoms (pain, constipation, sleep problems, nausea, vomiting, sedation, anxiety, and blackouts) in the younger age group and decreased in the older age group (≥ 65 years). As previously stated, literature on symptom prevalence among elderly patients with advanced cancer diagnosis is scarce. One important systematic review and meta-analysis published in 2014 by Van Lancker et al. [9] reported that fatigue, excretory problems, urinary incontinence, asthenia, pain, constipation, and anxiety were the most prevalent symptoms in this group of patients.
Wada et al. [19] concurred with the present study's conclusion that the prevalence of depression in younger patients was considerably higher than in elderly patients. These authors examined the relationship between cancer patients' depressive symptoms and their age. In this multicenter, cross-sectional study, it was discovered that depressive symptoms in cancer patients decreased with increasing age, while fatigue, dyspnea, and depression were substantially higher in younger patients.
In this study, it is crucial to note that the prevalence of the most prevalent symptoms was higher than reported in the majority of published literature. In the current investigation, the late referral of patients to palliative care is the most plausible explanation for the higher prevalence of symptoms. This is corroborated by the group's shorter overall survival (OS). This higher prevalence of symptoms in the current study indicates that the majority of patients referred to palliative care were at the end of life.According to numerous literatures, the PPS scores did not differ between the two age groups. The majority of patients lied between 30 and 40 percent of the PPS score. In their 2009 study, Lue et al. [20]categorized age as 45, 45 - 64, 65 - 74, and 75 – 84. These authors concluded that there were no statistically significant differences in PPS between age categories. In this study, older patients had a nonsignificantly longer median OS (20 days) than younger adults (16 days, p = 0.078). The short median OS in this study (17 days) has been previously reported by Hui D. et al. in 2010 [21]. Over the course of five years, they analyzed the median OS of 2,568 patients admitted to an acute palliative care unit. Their OS duration was 21 days (range: 19-23 days).
In this study, the most prevalent type of cancer in both age groups was gastrointestinal, followed by hepatobiliary. However, lung cancer was more prevalent in the elderly than in adults. There are no comparative investigations of cancer types between these two age groups. In their report on cancer statistics in the United States of America, Siegel et al [22] reached similar conclusions. From 2017 to 2019, the prevalence of all cancer categories increased by 61.2% among patients aged 70 and older. In this age group, lung cancer was the most prevalent, followed by colon and rectum malignancies. It is essential to note that the different races and ethnicities of the emigrant patients included in this current study were considered to be the primary determinants of their cancer type.
Conclusion
In conclusion, the present study confirmed a high symptom burden and prevalence among patients with advanced cancer diagnosis under the palliative care program. Tiredness, anorexia, drowsiness, pain, depression and anxiety were the most common prevalent symptoms with an incidence of >70%. Symptom prevalence were generally higher in younger adults compared to elderly patients especially pain, anorexia, anxiety and depression which were significantly higher in the younger age group (<65 years).
The short median OS (17 days) in the present study necessitates an earlier integration of palliative care in the overall management of patients with advanced cancer diagnosis in our center, irrespective of patients’ age upon referral to palliative care.
Conflict of Interest
No conflict of interest to declare.
Ethics Approval and Consent to Participate
The ethical approval has been obtained on 21st March 2022 from ethics committee of Medical Research Center in Qatar after completion of the ethical guidelines and regulation of Hamad Medical Corporation with reference ID MRC-01-22-034, but, the need of informed consent was waived as these are data for deceased patient in electronic medical record.
References
1. Sewtz C, Muscheites W, Grosse-Thie C, Kriesen U, Leithaeuser M, Glaeser D, et al. Longitudinal observation of anxiety and depression among palliative care cancer patients. Annals Palliative Med. 2021; 19(4): 3836-3846.
2. Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliative care. 1991; 7(2): 6-9.
3. HuiD,Bruera E. The Edmonton Symptom Assessment System 25 years later: past, present, and future developments. J pain symptom management. 2017; 53(3): 630-643.
4. Richardson LA, Jones G. A review of the reliability and validity of the Edmonton Symptom Assessment System. Current Oncol. 2009; 16(1): 53-64.
5. Prompantakorn P, Angkurawaranon C, Pinyopornpanish K, Chutarattanakul L, Aramrat C, Pateekhum C, et al. Palliative Performance Scale and survival in patients with cancer and non-cancer diagnoses needing a palliative care consultation: a retrospective cohort study. BMC Palliative Care. 2021 Dec;20(1):1-7.
6. Stone P, Vickerstaff V, Kalpakidou A, Todd C, Griffiths J, Keeley V, et al. Prognostic tools or clinical predictions: Which are better in palliative care?. PLoS One. 2021; 16(4): e0249763.
7. Omran S, KhaderY, McMillan S. (2017). Symptom clusters and quality of life in hospice patients with cancer. Asian Pacific jcancer prevention: APJCP. 2017; 18(9): 2387.
8. Dhingra L, Barrett M, Knotkova H, Chen J, Riggs A, Lee B, et al. (2018). Symptom distress among diverse patients referred for community-based palliative care: sociodemographic and medical correlates. J Pain Symptom Manag. 2018; 55(2): 290-296.
9. Van Lancker A, Velghe A, Van Hecke A, Verbrugghe M, Van Den Noortgate N, Grypdonck M, et al. Prevalence of symptoms in older cancer patients receiving palliative care: a systematic review and meta-analysis. J pain symptom manag. 2014; 47(1): 90-104. Retrieved from https://doi.org/10.1016/j.jpainsymman.2013.02.016
10. Webber K, Davies AN, Leach C, Waghorn M. Symptom prevalence and severity in palliative cancer medicine. BMJ Supportive & Palliative Care. 2021.
11. Kozlov E, Phongtankuel V, Prigerson H, Adelman R, Shalev A, Czaja S, et al. (2019). Prevalence, severity, and correlates of symptoms of anxiety and depression at the very end of life. Journal of pain and symptom manag. 2019; 58(1): 80-85. doi:10.1016/j.jpainsymman.2019.04.012
12. Olden AM, Holloway R, Ladwig S, Quill TE, vanWijngaarden E. Palliative care needs and symptom patterns of hospitalized elders referred for consultation. Jpain and symptom manag. 2011; 42(3), 410-418. doi:10.1016/j.jpainsymman.2010.12.005
13. Clark D. Total pain', disciplinary power and the body in the work of Cicely Saunders, 1958–1967. Social science med. 1999; 49(6): 727-736.
14. Hagarty AM, Bush SH, Talarico R, Lapenskie J,Tanuseputro P. Severe pain at the end of life: a population-level observational study. BMC palliative care. 2020; 19(1): 1-13.
15. Barbera L, Seow H, Howell D, Sutradhar R, Earle C, Liu Y, et al. Symptom burden and performance status in a population‐based cohort of ambulatory cancer patients. Cancer. 2010; 116(24): 5767-5776.
16. Cataldo JK, Paul S, Cooper B, Skerman H, Alexander K, Aouizerat B, et al. Differences in the symptom experience of older versus younger oncology outpatients: a cross-sectional study. BMC cancer. 2013; 13(1): 1-16.
17. Mohile SG, Heckler C, Fan L, Mustian K, Jean-Pierre P, Usuki K, et al. Age-related differences in symptoms and their interference with quality of life in 903 cancer patients undergoing radiation therapy. J geriatric oncol. 2011; 2(4): 225-232. https://doi.org/10.1016/j.jgo.2011.08.002
18. Kirkova J, Rybicki L, Walsh D, Aktas A. Symptom prevalence in advanced cancer: age, gender, and performance status interactions. AmJ Hospice Palliative Med. 2012; 29(2): 139-145. https://doi.org/10.1177/1049909111410
19. Wada S, Shimizu K, Inoguchi H, Shimoda H, Yoshiuchi K, Akechi T, et al. The association between depressive symptoms and age in cancer patients: a multicenter cross-sectional study. J Pain Symptom Manag. 2015; 50(6): 768-777.
20. Lau F, Maida V, Downing M, Lesperance M, Karlson N, Kuziemsky C. Use of the Palliative Performance Scale (PPS) for end-of-life prognostication in a palliative medicine consultation service. J pain symptom manag. 2009;37(6):965-72.
21. Hui D, Elsayem A, Palla S, De La Cruz M, Li Z, Yennurajalingam S, et al.Discharge outcomes and survival of patients with advanced cancer admitted to an acute palliative care unit at a comprehensive cancer center. J palliative med. 2010; 13(1): 49-57.
22. Siegel RL, Miller KD, WagleNS, Jemal A. Cancer statistics, 2023. CA: a cancer J for clinicians. 2023; 73(1): 17-48.
Received: June 05, 2023
Accepted: June 28, 2023
Published: June 30, 2023.
To cite this article : Abdullah H, Allam A, Al keldi S, Idris Z,Hassan A, Singh K, et al.A Comparative Study of Symptom Prevalence between Adults and Elderly Patients with Advanced Cancer Diagnosis Under Palliative Care: A Single Institution Experience. British Journal of Cancer Research. 2023; 6(1): 623-628. doi: 10.31488/bjcr.184.
© The Author(s) 2023. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/)
