Research Article / Open Access
DOI: 10.31488/bjcr.156
Cancer Treatment during the Sars-Cov-2 Pandemic: Single CenterAnalysis
Sowmica Devabhaktuni*1,P Jovita M. Martin Daniel*2,Kumanan.J,Ravichandran Ambalathandi*3,Manickavasagam Meenakshisundaram*4, Sharat Chandra Manikonda *5
1. Resident Medical Oncology,Department of Medical Oncology, SRMC, Chennai, Tamilnadu, India
2.Associate Professor Medical Oncology,Department of Medical Oncology, SRMC, Chennai, Tamilnadu, India
3. Assistant Professor medical Oncology,Department of Medical Oncology, SRMC, Chennai, Tamilnadu, India
4. Professor Medical Oncology, Department of Medical Oncology, SRMC, Chennai, Tamilnadu, India
5. Director Innodatatics, Hyderabad, India
*Corresponding author:1. Dr.P.Jovita M. Martin Daniel, Associate Professor Medical Oncology, SRMC,SRIHER, Porur, Chennai-116, Tamilnadu, India
2. Dr.Ravichandran Ambalathandi Assistant Professor Medical Oncology, SRMC,SRIHER, Porur, Chennai-116, Tamilnadu, India
Abstract
Objective: The Government of India under the ordinance of Prime Minister Narendra Modiimposed a nationwide lockdown on 24 March 2020, as a preventive measure against the COVID-19 pandemic in India; limiting movement of the entire 1.3 billion population of India. Hence the continuing cancer treatment posed a big challenge during the pandemic.There were several issues such as, lack of clear guidelines for cancer treatment during pandemic situation; unavailability of public transport; difficulty in getting e-pass; dread among the patients to access a health care facility and financial constraints during lock down. In this article, we reviewed the challenges faced and the measures taken to continue the cancer care during the COVID-19 pandemic and report the statistical analysis of patients treated with chemotherapy since the start of national lock down to September 2020.Methodology:In view of the national lock down which started in India, hospitals had to abate the elective patient care in all departments during the initial 6 months.In this article, we reviewed the retrospectively collected, statistical data of 522 inpatient admissions of various age groups, in our center in the department of medical oncology, on those who were treated with chemotherapy and other palliative care during this pandemic from March 24th 2020 to September 30th 2020. We also analyzed the problems faced by the patients during the lock down in order to access the health care so that the seamless management was provided to them amidst the pandemic. The decision of giving chemotherapy was determined by the performance status, the co morbiditiesand the intent of treatment, controllingthe disease burden which results in extension of life, patient's tolerance and patient’s covid-19 status before each cycle of chemotherapy. Results: As on September 30th India had 63, 10,264COVID-19 cases, Tamil Nadu had 5, 97,602 cases and Chennai being the hot spot had 1, 67,376 cases with 11,323 active cases. Despite the pandemic being a setback, we have treated 172 cancer patients, out of which 97 patients (56%) received neo adjuvant and adjuvant chemotherapy with curative intent and 58 patients (33%) received palliative chemotherapy with selected patients among them receiving growth factor support. Among the 172 patients, 8 patients (5%) tested positive for COVID-19 during or at start of the treatment, out of which 6 patients recovered and were restarted on cancer treatment and 2 succumbed to death. The PPV (positive predictive value) is 0.953 versus NPV(negative predictive value) 0.9943. The case fatality rate (CFR) in COVID with cancer patients was 2/8= 0.25 versus COVID-only patients 80/3107= 0.0257.Conclusion: The infectivity rate of COVID-19 was attenuated among the patients on cancer chemotherapy by adequate precautions; therefore the aftermath was not significant enough to delay the systemic treatment of cancer patients owing to COVID-19 pandemic situation.
Keywords:Cancer care in Pandemic times; COVID-19 Pandemic cancer treatment
Introduction
COVID-19 pandemic
COVID-19 pandemic has amended our modus vivendi. Along with all other aspects, the health care system did reach an abyss; in many countries it has taken a deep hit with lack of resources, proper guidelines and difficulty for patients to access the health care system. Distinctly, there has been a critical compromise in the cancer care in many centers. Studies from various countries showed that males had a higher percentage of death as compared to female counterparts [1-3].The impact was significant, due to the delay in diagnosis, chemotherapy, radiotherapy and surgery which has resulted in poor outcomes [3-5]. Various healthcare systems around the world have formulated their own strategies in controlling COVID-19 infection, andalso maintained the integrity of care for other illnesses including cancer [6]. In this article, we have reviewed the strategies undertaken at our centre to maintain the continuity of cancer care, data analysis about the cancer care during the pandemic and challenges we have faced during the process of providing healthcare.
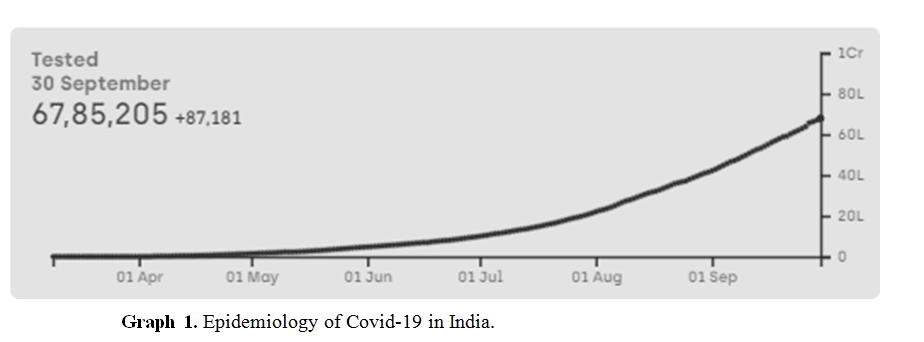
Epidemiology of Covid-19 in India
In India, the first COVID-19 case was reported on 30th January 2020.[7] On September 30th India had a total of 63,10,264 cases with 98,708 deaths(Graph 1) [8].
Methods
Data collection
This is a retrospective observational study of all the patients admitted from 24th March 2020 to 30th September 2020, conducted in the department of Medical Oncology in Sri Ramachandra Medical Institute of Higher Education and Research, Chennai, Tamil Nadu, India. Along with all basic details like age, sex, address; disease related data like site, chemotherapy details, need for supportive care were also collected. We also collected COVID-19 infection data in these patients.
Data analysis
The analysis of all basic characteristics was done using Microsoft Office Excel 2016 (Microsoft, Redmond, WA, USA) and the Normal probability calculation was done.
Results
Admissions for cancer treatment
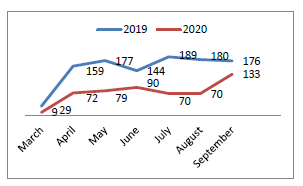
During the study period, we admitted a total of 172 patients with 522 admissions among them. There was almost 50% reduction (522 vs 1053) in total number of admission during the study period when compared to the number of admissions during the same period last year (Graph 2). Overall hospital has admitted 3107 patients with COVID19 only without cancer with 80 deaths during the same period.
Graph 2. Comparison between the number of admission from the period of March to September 2019 and 2020.
Patient characteristics
We treated patients of varying age groups with youngest being 24 years and oldest being 80 years. Most number of patients fell into the age group of 51- 60years (33%).We treated 51 patients (29%) above the age of 60 years, which was considered as high risk for severe COVID-19 illness [2]. Out of the 172 patients, 50 (29%) were males and 122 (71%) are females. Most of the patients were from Chennai City (74%). 25% patients were from other districts of the same state and 1% was from other states.
Table 1. Patient characteristics
| Number | Percentage (%) | |
|---|---|---|
| Gender | ||
| Male | 50 | 29 |
| female | 122 | 71 |
| Age | ||
| >60years | 51 | 30 |
| ≤60years | 121 | 70 |
| Region | ||
| Same district Other state | 122 | 74 |
| Other district from same state | 4 | 24 |
| Other state | 19 | 1 |
| Disease setting | ||
| Curative | 97 | 57 |
| Palliative | 58 | 34 |
| Biophosphonate | 15 | 9 |
| cancer diagnosis | ||
| Breast | 71 | 41 |
| Gastrointestinal System | 21 | 12 |
| Genitourinary | 6 | 0.03 |
| Gynaecological | 29 | 16 |
| Head and neck | 10 | 0.05 |
| Hematological | 13 | 0.07 |
| Lung | 16 | 0.09 |
| Others | 6 | 0.03 |
Majority of the patients treated had Breast as the primary site of cancer (71%) followed by gynecological cancers (29%) and cancers of gastrointestinal tract (21%). According to the intent of treatment, 57% were treated with a curative intent with either adjuvant or neo-adjuvant chemotherapy and 34% were treated with a palliative intent. 9% patients were admitted for bis-phosphonate administration as they were on aromatase inhibitors. Pegylated Filgrastim (PEG-CSF) support was given to 61 (35%) patients (Table 1).
Supportive care
When we compared this data with supportive care admission in the same months of 2019, we found that the supportive care admissions were higher last year than the current year. A total of 19 (3%) admissions out of 522 were for supportive care in the study period. During the same months of 2019, supportive care admissions were 63 (5.7%) out of 1053.
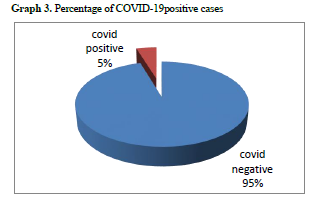
COVID19 positivity
Among the 172 patients who were on cancer treatment during the lockdown period, only 8 (4.6%) patients tested positive for COVID-19 RT-PCR. Out of these 8 patients, 2 patients expired during the treatment for COVID-19. However, the cause of death was uncertain as they also had advanced malignancy and multiple co-morbidities. The rest of them recovered from the COVID-19 infection without any disease related morbidity and were restarted on chemotherapy.They had no complications with subsequent chemotherapy. [Graph 3] The stat (%) admission (in-patient vs. out-patient) 2020 IP vs OP =1058/2683= 0.394 (40%); 2020 IP vs OP =522/1324=0.394 (40%). The PPV (positive predictive value) is 0.953 versus NPV 0.9943. The case fatality rate (CFR) in COVID with cancer patients was 2/8= 0.25 versus COVID-only patients 80/3107= 0.0257.
Discussion
A substantial proportion of patients diagnosed with cancer have an 'aggressive disease', which is reflected through a short time of progression or lack of disease control amidst treatment in some cases. The clonogenically potent stem cell follows the Gompertizian curve in logarithmic growth or cell kill[9]. Hence, maintaining the dose intensity and duration is mandatory for a proper yield of results. However in a pandemic situation like the COVID-19, we are forced to under dose patients, postpone treatments and substitute chemotherapeutics with simple economical oral metronomic chemotherapy drugs or hormonal agents or oral small molecules as per the histology and site requirements. The initial months of COVID-19 had a large impact on the decision making of the Oncology patients due to the exaggerated fear factor. We were rather too cautious, as we were not aware of the infectivity rate or pattern of spread. Hence, a vast majority of the Oncology patients deferred from the routine schedule of chemotherapy /radiotherapy/ surgery. It is indeed needless to mention that those with advanced age, frail immune system and multiple uncontrolled co-morbidities will fall out of the purview of immune compromising chemotherapy. Whilst we should tangibly remember the oath of non-maleficence by the Hippocrates, we need to weigh the COVID-19 over the aggressiveness of the cancer itself. Eventually once the COVID-19 resolves, we will land up with converting our intent from all potentially curable intent to palliative intent for patients or even worse just a terminal supportive care, due to inadequate timely treatment or postponement of treatment lacking the dose intensity of chemotherapeutics.
In our study,the case fatality rate in COVID with cancer patients 0.2% versus COVID-only patients 0.0257%was assessed in our study is comparable to the COVID with Cancer survivors versus the COVID only patients with co-morbidities in the other literature review. However the case fatality rate in COVID-19 with Cancer was very less 0.2% in our study versus 37 % maximum as mentioned in the literature [10-15].This disparity was probably due to the tropical climate and the stringent precautions adopted. This in turn translated to lower death rate in the COVID-19 cancer patients as against the high case fatality mentioned in the literature[10-15].
The measures taken to tackle COVID-19 infection
(i) By the Government were
• Lockdown imposed in the Country
• Creating e-pass system thereby allowing only people with important conditions to cross cities or state borders.
• Creating awareness through media.
• Camps were held in every street to pick up COVID-19 Cases.
(ii) By the hospital were,
• Thermal screening of all patients entering the hospital.
• Restricting the number of attenders
• Washing hands often with soap and water for 20 seconds or more (use hand sanitizer with at least 60% alcohol in the absence of water)
• Patients were advised to refrain from touching your eyes, nose or mouth
• Patients were advised to refrain from contact with people, especially those who are sick
• Patients were advised to cover mouth and nose with a tissue/ handkerchief / sleevewhen coughing or sneezing, and then discard the tissue ( wash the handkerchief/ clothes soiled)
• Patients were advised to clean and disinfect touched objects and surfaces frequently using a regular household cleaning spray or wipe
• Patients were advised to exercise appropriate social distancing
(iii) From the Health Care professionals (HCP) side
• PPE kits were used
• Rotation of duties in Medical Oncology to avoid all HCP being exposed on the same day.
• Restricting the entry of patient bystanders ( only one attender allowed at a time , the attender is allowed to talk to the HCP sequentially after the patient leaves the room essentially permitting only one person to enter the HCP’s room)
(iv) Modifications in patient management during COVID-19
• COVID-19 tests were made mandatory to all patient and bystanders.
• Old, Frail patients or those with multiple co-morbidities were asked to refrain from hospital visits and Intravenous (IV) chemo.
• Tele-consults were encouraged an interim change of chemo to oral chemo /hormonal agents were given for those as a stop-gap resort.
• All Patients with IV chemo were given liberal growth factor supports.
• If patient was detected COVID-19 until he/she turns COVID RT-PCR negative and proper evaluation of the performance and the recovery of the patient from COVID-19 , they were not called in for IV chemo.
Compared to 2019 and 2020, the number treated cases have decreased in hospitals albeit the mortality was almost the same due to COVID-19. This could also be due to the right choice of selecting the fit patients for chemotherapy and leaving the rest for oral metronomic chemotherapy/ hormonal treatment/ small molecule inhibitors. This difference in number of patients attending their outpatient consultations was majorly influenced by fear of accessing health care system by patients during a pandemic, practical difficulties like lack of public transport, stringent protocols in obtaining e-pass, temporarily withheld surgical oncology procedures and initial hesitancy in giving cancer chemotherapy especially for hematological malignancies and metastatic solid tumors due to paucity of literature and evidence of treating patients with chemotherapy during a virus pandemic. One other reason for decreased admissions during lockdown is the unavailability of public transport and restrictions imposed by the government on travelling. Even though government started issuing e-passes later, obtaining them was a hassle. People travelling from other states had the additional difficulty of staying in quarantine facilities for 14 days on arrival.
One size never fits all. In the bargain of controlling infection, denying treatment of a potentially curable malignancy will result in loss of a life to cancer in the future if not to COVID-19 immediately. Therefore treatment should be highly individualized. The Risk versus benefit ratio is accounted for an unbiased decision making. In substantial number of cases, the benefits of treatment take precedence over the risks of delaying or stopping therapy. There are equally other situations in which delaying or rescheduling treatment is possible. Furthermore, it depends on the type of cancer, the treatment, co-morbidities, performance, affordability of resources and of course the patient’s preference. Patients should talk with their oncologist to determine the best individualized treatment plan for them [15,16].
With proper precautionary methods and stringent rules, we were able to maintain the integrity of proper safe treatments and the results. Our study showed the appropriate fit individuals could tolerate the chemotherapy well under proper precautions in COVID-19 pandemic. Many unfit, frail and older patients were followed up remotely with oral metronomic regimens, hormonal treatment and small molecules without much issue [15-17].
Conclusion
Cancer growth isn’t going to wait for COVID-19 pandemic to resolve. We have been adopting very strict preventive measures in hospitals at all levels in the current situation. This style of operation, as attenuated the outcome (CFR in our study in comparison to the CFR in COVID-19 in cancer patients mentioned in the literature) and has yielded us safety from infections and good results for patients on chemotherapy[10-15]. Extrapolating the current study data and experience it is apparent that we may unswervingly render appropriate cancer treatment strategies (remotely or in person) to patients not compromising on the cancer care at any level. The ultimate aim is that, we may have a seamless management of cancer care even during COVID-19 pandemic situations with better results not denying of the worthy patients their timely interventions, with individual tailor made decisions.
Acknowledgements
We acknowledge the Medical Records team, staff nurses, the administration (Mrs.Francina Mala) and reception team (Mrs.Nalini and Ms.Deepika) for all the efforts and contribution.
Conflicts of Interest
NIL
References
1. Jeffrey G, Kai S. Modi Orders 3-Week Total Lockdown for All 1.3 Billion Indians. The New York Times. ISSN 0362-4331, 2020.
2. Wu Z, McGooganJM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323(13), 1239–1242.
3. Richardson S, Hirsch JS, Narasimhan M, et al (2020). Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020; 323(20), 2052–2059.
4. Kuderer NM, Choueiri TK, Shah DP, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020; 6736 1–13.
5. Sud A, Jones M, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020; 13:19.
6. Anderson RM, Heesterbeek H, Klinkenberg D, et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020; 395 931–934.
7.COVID19 pandemic in India. Wikepedia.2020.
8. https://www.covid19india.org
9.Kendal WS. Gompertzian growth as a consequence of tumor heterogeneity. Mathematical Biosciences. 1985; 73:103-107
10.Curigliano G. Cancer Patients and Risk of Mortality for COVID-19. Cancer Cell. 38: 2020
11.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21: 335–337.
12.Miyashita H, Mikami T, Chopra N, et al.(2020). Do Patients with Cancer Have a Poorer Prognosis of COVID-19? An Experience in New York City. Ann Oncol. 2020.
13.Karotia D, Kumar A.A Perspective on India’s Fight against COVID – 19. Special Issue on SARS-CoV-2 (COVID-19). Epidemiol Int. 2020;5: 22-28
14.Kuderer NM, Choueiri TK, Shah DP, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. The Lancet. 2020; 395: P1907–P1918.
15.Mehta V, Sanjay Goel S, Kabarriti R, et al. Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System . Cancer Discov.2020;10(7):935-941.
16.https://healthcare-in-europe.com/en/news/covid-19-could-cause-20-rise-in-cancer-deaths.html
17.https://cinj.org/patient-care/covid-19-what-cancer-patients-need-know
Received: June 10, 2020.
Accepted: June 19, 2020.
Published: June 26, 2020.
To cite this article : Sowmica D, Jovita MD, Kumanan J, et al. Cancer Treatment during the Sars-Cov-2 Pandemic: Single Center Analysis. British Journal of Cancer Research. 2020; 3:4..
© Jovita MD, et al. 2020.
