Case Report / Open Access
DOI: 10.31488/bjcr.173
Dermatofifibrosarcoma Protuberans of Vulva. A Rare and Diffifficult Case
Joshua Dean M.D*1, Jill Gadzinski M.D2, Zaid Al-Wahab M.D2
1. Department of Obstetrics and Gynecology, Beaumont Health, Roy al Oak, MI, USA
2. Department of Gynecology Oncology, Rose Cancer Center/Beaumon t Health, Royal Oak, MI, USA
*Corresponding author:Joshua Dean M.D, Department of Obstetrics and Gynecology, Beaumont Health, Royal Oak, MI, USA
Abstract
This case report highlights a unique patient presentation of a rare form of vulvar cancer, dermatofibrosarcoma protuberans (DFSP). Due to DFSP’s rarity for vulvar presentation, most gynecologists and gynecologic/oncologists do not encounter this disease in their careers. There can be significant difficulty in identifying this lesion, for both the patient and primary provider, resulting in a delay in care and limitations management. Our patient, was a 60-year-old female whom had a delayed presentation to a gynecologic oncologist given her limited primary gynecologic follow up. She developed a 1.8cm vulvar lesion, which was positive for CD34 staining that confirmed the diagnosis of DFSP. Her management entailed a wide local excision of the lesion with a goal of 2 cm negative margins. She has followed up 3 years postoperatively without disease recurrence. There are a limited number of publications that detail the presentation, management and surveillance of DFSP. The objective of this case report is to discuss a patient’s presentation, disease course, management and post-treatment surveillance plan in order to help oncologists and gynecologists manage this rare disease.
Key words: Dermatofibrosarcoma Protuberans, Vulvar Cancer, CD34 staining
Introduction
Dermatofibrosarcoma protuberans (DFSP) is a rare and disabling malignancy. It arises as a lesion consisting of small nodules that progress to a large ulcerative tumor with a high potential for local invasion. Often this tumor has low metastatic potential. However, there is a large risk for recurrence given its deep infiltrative growth pattern and a difficulty to resect to negative margins. Patients typically present between their fourth to sixth decade of life [1]. Trunk, head or neck involvement is most common [2]. Rarely, this lesion can present at the vulva reflected with less than 60 cases reported in the literature [3].
The pathogenesis of this neoplastic lesion arises from a translocation of chromosomes 17 and 22 or chromosomes 22 and 13, which leads to the fusion of collagen type 1alpha 1 protein and platelet derived growth factor subunit beta proteins (PDGFRB). This fusion results in a continuous activation of the PDGFRB receptor, enhancing mitosis of mesenchymal cells leading to significant cell proliferation [1, 2]. Pathologically, it is a fibrous tumor of low-intermediate grade malignancy that arises from fibroblasts within the dermal connective tissue layer of the skin [4- 6].
Patients often present with an initial complaint of a chronic vulvar lesion that has slowly increased in size. The initial presentation can coincide with an onset of ulceration and bleeding from the lesion. Patients may also present with vulvar and thigh discomfort, and dyspareunia [4,5,8]. Previous studies reveal that there are no significant risk factors. However, the average patient presentation is a woman in her fourth through sixth decade of life [1, 8, 9] and more common in black Americans compared to other ethnicities [10]. An awareness of vulvar health by gynecologists during yearly annual visits can help identify these lesions earlier in order to improve overall surgical outcome.
DFSP has an incidence of 3.2 per 1 million [7] for all anatomic locations, with vulvar presentation being a very rare subset of this malignancy [4, 8, 9]. Therefore, limited information is available on the management and prognosis of vulvar DFSP. This is evident with no standard staging system established for prognosis [2]. It is not unexpected that patients may delay presentation to a primary provider or primary providers may delay referral to a gynecologic oncologist. Primary providers may not be apt to include this disease in a differential diagnosis, potentially leading to a delay in treatment and worse outcomes [7]. This case report is presented to aid providers in the recognition and management of DFSP.
Case Presentation
Our patient presented at 60 years of age to her primary gynecologist with a complaint of dyspareunia for 6 months. She had limited gynecologic follow after she underwent a total hysterectomy with bilateral sapling-oophorectomy in 2004. She initially attributed her dyspareunia to be secondary to genitourinary syndrome of menopause. However, she soon developed a right labial lesion that progressively increased in size. This lesion was eventually biopsied by her gynecologist. Biopsy results came back positive for CD34 staining (Figure 1), confirming the diagnosis of DFSP. She was referred to gyn-oncology for management. Preoperative imaging with MRI revealed no discrete mass, lymphadenopathy or sign of metastatic spread (Figure 2).

Figure 1:Tumor with CD34 staining at 20x magnification

Figure 2:Preoperative MRI revealing no identifiable lesion, local invasion or metastatic spread
She underwent a radical excision of her right vulva with 2cm margins. Intraoperatively, her lesion was 1.8cm by 1.5 cm in size. Pathology revealed a grade 1 lesion with <2 mitoses per high power field, absent necrosis and positive surgical margins. Her histology revealed the classic findings of spindle configuration (Figure 3) and papillary infiltration by the tumor cells (Figure 4).
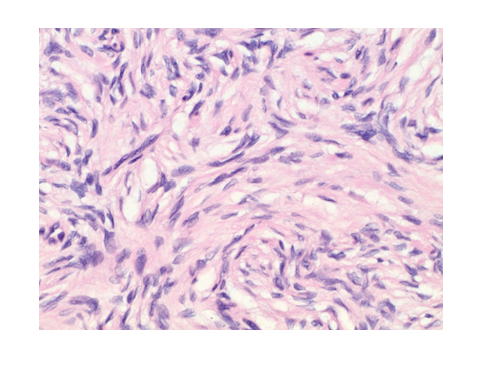
Figure 3:Tumor spindle cell configuration stained with hematoxylin and eosin at 400x magnification
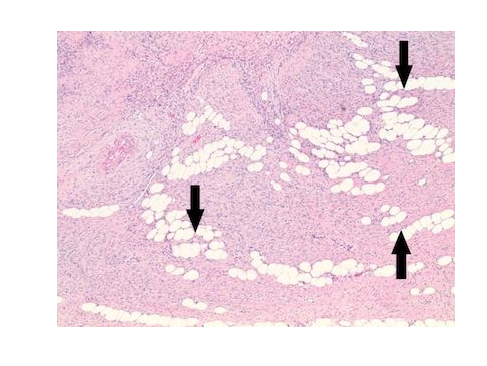
Figure 4:Tumor finger-like projections (arrows) stained with hematoxylin and eosin at 40x magnification
Three months following index surgery, our patient underwent a repeat excision at the region of positive surgical margins. Pathology from the re-excision revealed no residual neoplasm. The patient established a plan to follow up with gyn-oncology every 3 months for vulvar and pelvic exams. She was also recommended to have repeat MRI exams every 6 months in her first three years of surveillance. Three years from her index surgery, our patient has remained without signs of recurrent disease.
Discussion
Dermatofibrosarcoma protuberans has a rare propensity for primary vulvar involvement. A delay in diagnosis and management may pose difficulty in achieving remission or preventing recurrence. It is critical that general practitioners, gynecologists and oncologists are well aware of the identification and appropriate management of this vulvar malignancy.
Initial evaluation with a biopsy is crucial for diagnosis. CD34 staining is diagnostic of DFSP (Figure 1) [5, 9]. Classic histology reveals a storiform pattern of spindle cells (Figure 2) extending from the reticular dermis to subcutaneous layer with finger like projections with pleomorphic vesicular nuclei (Figure 3) [4]. Tumor cells have an average mitotic index of <4/10 per HPF [4, 8, 9]. When there is a loss in these histologic features, there is a concern for fibrosarcomatous transformation. This is a sign of an increased risk of local recurrence or metastasis [3].
Standard management for DFSP is surgical resection. Prior to surgical intervention, a preoperative CT or MRI is critical for surgical planning and to evaluate for metastasis. At our institution, we proceeded with a radical excision to 2 cm negative tumor margins. This technique is well published in the literature [3- 6, 8]. However, given its propensity for local infiltration, there might be difficulty in surgical resection. An alternative surgical approach relies upon mohs micrographic surgery given its ability for intraoperative evaluation of margins utilizing frozen section. Significant resources are utilized for this procedure and it is not an ideal approach for large lesions [7].
Therapeutic options have been evaluated in the literature for patients at risk of recurrence or suboptimal tumor resection. Imatinib, a tyrosine kinase inhibitor, has been described at a dose of 400-800mg/d as a suitable option for neoadjuvant therapy or primary therapy for patients with inoperable lesions (11, 12). In patients at high risk of recurrence, Du et al. described radiation therapy at a dose of 50-60 Gy at 2 Gy/fraction for 5 fractions/week as successful approach at achieving a disease free survival of 94.6% at 3 years and 89.8% at 5 years [13].
Our patient presented with DFSP localized to her right vulva. Given that her preoperative imaging revealed no signs of extensive invasion or metastasis, a radical excision was performed. The decision was made to perform a re-excision in order to achieve negative surgical margins. Since our patient’s tumor histology was low risk for fibrosarcomatous transformation, there were no signs of metastasis on imaging and she ultimately had negative surgical margins, our team recommended surveillance at six-month intervals. The most common window of recurrence is within 3 years of initial surgery [2]. Three years since surgical intervention, our patient has remained in remission.
Conclusion
This case report highlights a rare patient presentation of DFSP at our institution. Our patient underwent a biopsy of a suspicious lesion prior to intervention, which revealed the histologic diagnosis of DFSP with CD34 staining. She had imaging prior to intervention in order to stratify her risk of metastasis. The intervention entailed an excision to 2-centimeter negative margins. Given difficulty with vulvar resection, reexcision was required for negative margins. This case report exemplifies the importance of close primary gynecology follow up with annual vulvar exams in order to identify lesions earlier for optimal prognostic outcome.
Abbreviation
DFSP: Dermatofibrosarcoma Protuberans
Conflicts of Interest
All the authors; Joshua Dean, Jill Gadzinski, and Zaid Al-Wahab; declare no conflicts of interest
References
1. Allen A, Ahn C, Sangueza OP. Dermatofibrosarcoma Protuberans. Dermatol Clin. 2019; 37 (4): 483-488.
2. Acosta AE, Velez CS. Dermatofibrosarcoma Protuberans. Curr Treat Options Oncol. 2017; 18 (9):56.
3. Jeremic J, Stefanovic A, Jeremic K, et al. Giant Dermatofibrosarcoma Protuberans Vulvae: Rare Clinical Presentation and Literature Review. J BUON. 2019; 24(3): 1289-1295.
4. Moodley M, Moodley J. Dermatofibrosarcoma Protuberans of the Vulva: A Case Report and Review of the Literature. Gynecology Oncology. 200; 78 (1), 74-75.
5. Soergel TM, Doering DL, O’Connor D. Metastatic Dermatofibrosarcoma Protuberans of the Vulva. Gynecologic Oncology. 1998;71 (2), 320-324.
6. Paramythiotis D, Stravrou G, Panagiotou D, et al. Dermatofibrosarcoma Protuberans: A Case Report and Review of the Literature. Hippokratia. 2016; 20(1):80-83.
7. Neff R, Collins R, Backes F. Dermatofibrosarcoma Protuberans: A Rare and Devastating Tumor of the Vulva. Gynecol Oncol Rep. 2019; 28: 9-11.
8. Nguyen AH, Detty SQ, Gonzaga MI, et al. Clinical Features and Treatment of Dermatofibrosarcoma Protuberans Affecting the Vulva: A Literature Review. Dermatol Surg. 2017; 43(6): 771-774.
9. Edelweiss M, Malpica A. Dermatofibrosarcoma Protuberans of the Vulva: A Clinicopathologic and Immunohistochemical Study of 13 Cases. Am J Surg Pathol. 2010; 34 (3): 393-400.
10. Veronese F, Boggio P, Tiberio R, et al. Wide Local Excision vs. Mohs Tubingen Technique in the Treatment of Dermatofibrosarcoma Protuberans: a two-centre Retrospective Study and Literature Review. J Eur Acad Dermatol Venereol. 2017; 31(12): 2069-2076.
11. Rutkowski P, Debiec-Rychter M, Nowecki Z, et al. Treatment of Advanced Dermatofibrosarcoma Protuberans with Imatinib Mesylate with or without Surgical Resection. JEADV. 2011; 25:264-270.
12. Merlo G, Cozzani E, Comandini D, et al. Neoadjuvant Imatinib as Treatment Preceding surgery for Vulvar Dermatofibrosarcoma Protuberans. Dermatol There. 2021; 34(2): e14860.
13. Du K, Li J, Tang L, et al. Role of Postoperative Radiotherapy in Dermatofibrosarcoma Protuberans: A Propensity Score-Matched Analysis. Radiat Oncol. 2019; 14(1):20.
Received: January 03, 2022;
Accepted: February 07, 2022;
Published: February 07, 2022.
To cite this article : Dean J, Gadzinski J, Al-Wahab Z. Dermatofibrosarcoma Protuberans of Vulva. A Rare and Difficult Case. British Journal of Cancer Research. 2022; 5(1): 540- 543. doi: 10.31488/bjcr.173.
©2022 Joshua Dean, et al.
