Case report / Open Access
DOI: 10.31488/bjcr.200
Surgical Treatment For Locally Advanced Vaginal Cancer Associated With Total Utero-Vaginal Prolapse
Cosima V.M. Brucker, Dimitrios I. Bolovis
University Women’s Hospital, Paracelsus Medical University, Nuremberg, Germany
*Corresponding author: Cosima V.M. Brucker. University Women’s Hospital, Paracelsus Medical University, Nuremberg, Germany
Abstract
Vaginal cancer is a rare gynecologic malignancy, accounting for 1-2% of gynecologic cancers. The most common type is squamous cell carcinoma. Typical symptoms of vaginal carcinoma include vaginal bleeding or discharge and pelvic pain. It occurs typically in women over 60 years old. In this population, pelvic organ prolapse occurs with increasing frequency, and therefore, the two entities may present synchronously. While there are clear standards for the therapy of vaginal cancer, the synchronous presentation of vaginal carcinoma with total prolapse requires broad knowledge in gynecologic oncology as well as in urogynecology. Radiation treatment can be challenging in untreated total prolapse due to the changes in anatomy, and the application of brachytherapy is not an option in cases when repositioning of the prolapse is not possible. Therefore, surgical removal of the tumor with simultaneous correction of the prolapse is the method of choice, followed by further treatment with radiation and/or chemotherapy as indicated. The surgical approach for removal of the tumor as well as simultaneous pelvic floor reconstruction needs to be planned thoroughly aiming at complete removal of tumor tissue and at the same time a reconstruction strategy facilitating subsequent radiotherapy and follow-up. Here we describe step by step a mesh-free approach which enables complete resection of cancer tissue followed by reposition of the prolapsed organs and plastic reconstruction of the vulva and vagina. The final result shows a normal pelvic floor anatomy, leading to high patient satisfaction.
Introduction
Pelvic organ prolapse (POP) is a condition that affects many women with increasing age. The clinical finding is a protrusion or herniation of the pelvic organs through the vaginal walls and pelvic floor.
The reported prevalence of POP varies according to different studies and is found to be anywhere between 3% and 50% [1-2]. These wide variations are due to differences in study design, inclusion criteria, and accompanying indicator symptoms used among studies. Within this common condition, the simultaneous occurrence of gynecologic cancer is possible. While endometrial and cervical cancer are encountered with an incidence of 10-25 cases per 100,000 women per year depending on ethnicity and country, vaginal cancer is much less frequent-with an incidence of 0.6 to 1.0 cases per 100,000 women per year. [3-4]. Consequently, the co-occurrence of vaginal cancer with POP is a very rare clinical finding. In a recent review, a total of 27 patients was identified in 21 studies [5].
Vaginal cancer occurs most frequently in women over 60 years old. Nearly 90% of the cases present as squamous cell carcinoma. 75% of the cases are related to HPV infection. Infrequently, adenocarcinoma, melanoma and also sarcoma may be diagnosed. Usually, symptoms include vaginal bleeding, dysuria and pelvic pain.
For the sporadic finding of total prolapse associated with vaginal cancer, treatment may be challenging. Possible treatment options include surgery, radiation therapy and radiochemotherapy (4). In general, treatment of vaginal cancer is associated with significant complications such as fistula, stricture, cystitis or proctitis. Fistula development independent of treatment modality was reported in 21% of patients in a large chart review study [6].
Surgical treatment is of particular interest in the case of concomitant prolapse, because it has the potential to remove the vaginal cancer and at the same time to restore normal anatomy and normal voiding function. Planned surgery for vaginal cancer should aim at complete tumor resection while at the same time providing a strategic plan for pelvic floor reconstruction. Several approaches have been proposed, in recent years also including prolapse correction with non-absorbable mesh. However, transvaginal prosthetic-free procedures including non obliterative techniques have shown some advantages compared with mesh augmentation, including lower costs and morbidity. Here we describe the basic principle of the surgical approach step by step on a large vaginal cancer associated with total prolapse, addressing both the oncologic as well as the urogynecologic aspects. A mesh-free approach with reposition of the prolapsed organs and anatomical reconstruction of vulva and vagina was chosen.
Case presentation
The 79-year-old caucasian patient G1P1 presented in our emergency department because of total prolapse, vaginal bleeding and odorous discharge. Gynecologic examination revealed a stage IV total prolapse according to the Pelvic Organ Prolapse Quantification system [7] with a large tumor on the posterior vaginal wall, measuring about 15 cm in diameter. The patient reported long standing prolapse over 30 years.
Her medical history included atrial fibrillation, arterial hypertension, diabetes mellitus, and chronic renal insufficiency. She was on medication with DOAK (Apixaban), Torasemid, Chlortalidon, Bisoprolol, Ramipril, Amlodipin, Sitagliptin, Metformin, Insulin and Pantoprazol. Appendectomy was the only previous surgery.
Her blood test revealed severe leukocytosis (30.3/nl) as well as anemia (Hb 9.2 g/dl). Retention parameters were elevated (urea 55 mmol/l, creatinine 1.28 mg/dl).
The patient was admitted to the gynecologic department with suspicion of vaginal cancer and total prolapse. A transurethral catheter was placed. Urinary tract infection was diagnosed and the patient received Cefuroxim and Metronidazole. Ultrasound of the bladder and kidneys showed an empty bladder with transurethral catheter in place and regular kidneys without retention. Reposition of the everted vagina was not possible. A biopsy from the vaginal tumor was taken, and histologically confirmed the tumor as moderately differentiated squamous cell carcinoma of the vagina with focal ulceration.
The patient underwent tumor staging, without any sign of metastasis or lymph node involvement. Primary surgical tumor treatment was indicated. The patient did not consent for surgical lymph node staging contrary to physician’s advice. Therefore, a subtotal colpectomy with hysterectomy, BSO and modified colpocleisis was scheduled.
The preoperative examination shows total prolapse with complete vaginal eversion. The tumor is located on the posterior wall with several satellite metastases (Fig. 1).
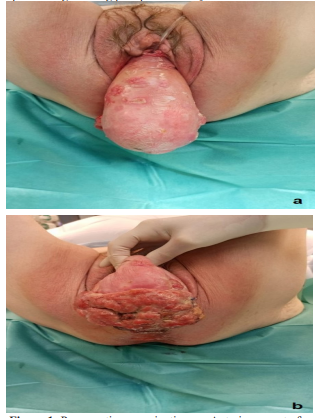
Figure 1:Preoperative examination. a : Anterior aspect of total prolapse with satellite metastases. b. Posterior aspect of total prolapse with large vaginal tumor.
Surgical method
A circular incision located 3 cm distally from the external ostium of the urethra defines the vaginal epithelium to be spared for vaginal reconstruction (Fig. 2a). Subsequently, vaginal flaps are prepared in order to perform the colpectomy. (Fig. 2b, 2c)
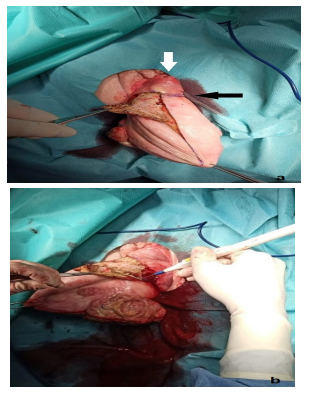
Figure 2:Surgical approach a The proximal resection line is defined 3cm from the external ostium of the urethra White arrow: external urethral ostium.Black arrow: proximal resection line. b Colpectomy using monopolar diathermia.

Figure 2c:Anterior flaps fully prepared. The cervix is grasped with tenaculum forceps (black arrow). White arrow: urethra.*de-epitheliated anterior compartment
In this case, the posterior flaps encompassed the tumor completely, with a macroscopic safety margin of at least 2 cm. The posterior vagina was resected en bloc with the pouch of douglas. This step allowed for digital control of complete tumor resection. The douglas peritoneum was left with the specimen (Fig. 2d, 2e). Following colpectomy and tumor resection, vaginal hysterectomy with BSO was performed (Fig. 2f).
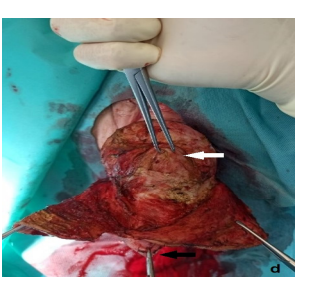
Figure 2d:Posterior flaps partially prepared. The amputated cervix remains with the specimen (black arrow). The cervical stump is grasped with tenaculum forceps (white arrow)
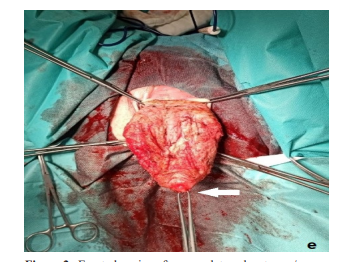
Figure 2e:Everted vagina after complete colpectomy / tumor resection White arrow: cervical stump.
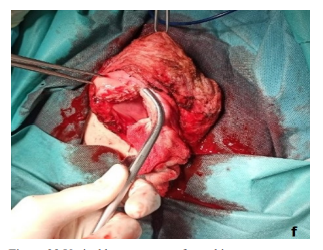
Figure 2f:Vaginal hysterectomy of atrophic uterus.
The intraoperative demonstration of the specimen shows macroscopic R0 resection with broad safety margins (Fig. 3a, 3b).
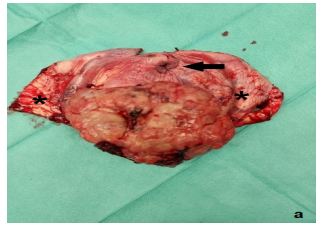
Figure 3a:Specimen with anterior flaps and tumor on the posterior vaginal wall.Black arrow: amputated cervix.*anterior flaps
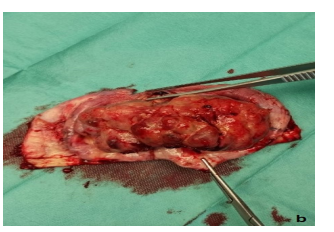
Figure 3b:Specimen demonstrating in sano resection with wide macroscopic safety margins anatomical reconstruction
For the reconstructive part, we performed a high circular peritoneal closure using Vicryl #0. Several purse string sutures were applied to push the bladder and rectum back to their normal positions and to reinforce the fascia under the vaginal wall using PDS 2x0. The vaginal epithelium was closed vertically using Vicryl #1 running sutures (Fig. 4a). In order to reduce the hiatus, we performed a posterior repair including a high perineoplasty (Fig. 4b). The reconstruction resulted in a physiologic anatomical appearance of the vulva and vagina with a vaginal length of approximately 8 cm. Total operation time was 129 min.
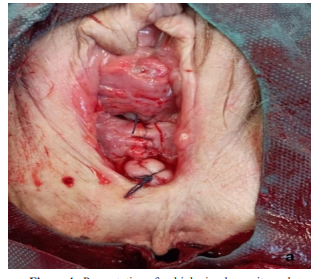
Figure 4a:Presentation after high circular peritoneal closure, fascia plication and vertical closure of vaginal

Figure 4b:Presentation after reconstruction of vulva, introitus and perineum.
Histological result and follow-up
The final histology result described a G3 vaginal cancer of 140 x 140 x 21 mm, pT2 L0 V0, FIGO II, since the tumor reached the underlying peritoneum of the pouch of douglas. The uterus was free of cancer with atrophic endometrium. Adjuvant radiochemotherapy was recommended by the interdisciplinary tumorboard following international guidelines.
After 3 months, the patient returned for a follow-up examination. She was free of tumor with normal anatomy. Gynecologic examination demonstrates a physiologic appearance of vulva and vagina (Fig. 5a, 5b). Patient satisfaction was very high.

Figure 5a:Natural appearance of vulva and introitus.
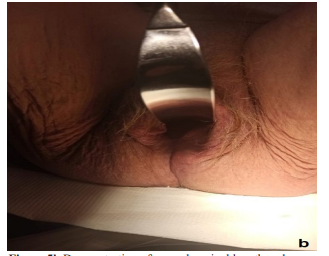
Figure 5b:Demonstration of normal vaginal length and width by insertion of Breisky speculum.
Discussion
The occurrence of primary carcinoma of the vagina is rare, usually affecting elderly women [8]. Given the rarity of vaginal cancer, studies about diagnosis and treatment of this tumor entity are limited to retrospective case series, usually from single-referral institutions. Treatment is always challenging, and the general options include radiotherapy, surgery, radiochemotherapy or palliative treatment [4]. The occurrence of vaginal cancer with irreducible uterine prolapse is a rare presentation, and this condition may cause difficulty with existing treatment protocols.
As with other cancer types, the treatment strategy for vaginal cancer is determined by the stage and location of the tumor. Patients with stage I vaginal cancer may be cured by surgical therapy only [9]. In stage II patients, usually a combination of EBRT and brachytherapy is applied due to frequent involvement of the parametrium [9]. In the case of vaginal cancer associated with total prolapse however, there is no pelvic sidewall involvement which is otherwise typical for vaginal cancer. Therefore, this condition is very amenable to a surgical approach even with larger tumors, since the entire malignant tissue is located outside of the pelvis.
Standard radiotherapy usually is administered as external beam radiation therapy (EBRT) and brachytherapy (BT). Vaginal BT is typically associated with fewer side effects compared with EBRT, however it is not feasible in a case with total vaginal eversion.
EBRT is associated with significant risk especially in the presence of associated total prolapse, because organs such as the bladder or bowel may be included in the cystocele or enterocele sac and thus more exposed to radiation. This can increase the likelihood of associated severe complications such as vesicovaginal or enterovaginal fistula. Therefore, when EBRT is administered, reduction of uterine prolapse and hysterectomy have been recommended before EBRT to reduce the risks of visceral injury and organ fistulas [10-11].
A surgical approach aiming at R0 resection of the tumor and at the same time at correction of the prolapse is advantageous in several ways. Firstly, it offers the chance for complete removal of the cancer. Secondly, it enables application of radiotherapy without elevated risk due to the anatomical reconstruction of the pelvic floor with re-positioning of vagina, bladder and bowel. Thirdly, it alleviates the psychologic and physical burden associated with total prolapse. And finally, it normalizes bowel and bladder function.
In this paper, we demonstrate modified colpocleisis as a suitable technique to address vaginal cancer associated with a high volume total prolapse. The technique can be applied also with low volume prolapse with and without the presence of vaginal cancer [12]. We use the term „modified“ because our technique not only avoids total closure of the vagina, but also includes reconstruction of a normal anatomy. As a result, standard radiotherapy can be applied following surgery. The avoidance of mesh material further contributes to a low morbidity profile. This way, high patient satisfaction can be achieved.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are noch publicly available due to privacy and ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.Funding statement
The authors received funding from the Johann und Maria Künast Foundation.
Acknowledgments
The authors are sincerely grateful to the patient for giving permission to share this informative case report.
References
1. Tegerstedt G, Maehle-Schmidt M, Nyrén O, Hammarström M. Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:497-503.3
2. Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Pelvic Floor Disorders Network. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300:1311-6. 4.
3. Wu X, Matanoski G, Chen VW, Saraiya M, Coughlin SS, King JB, et al. Descriptive epidemiology of vaginal cancer incidence and survival by race, ethnicity, and age in the United States. Cancer. 2008 Nov 15;113(10 Suppl):2873-82.
4. Diagnosis, Therapy and Follow-Up Care of Vaginal Cancer and its Precursors. Guideline of the DGGG and OEGGG (S2k-Level, AWMF Registry No. 032/042, October 2018.
5.Frigerio M, Inzoli A, Barba M. Pelvic organ prolapse and vaginal cancer: A systematic literature review. Int J Gynaecol Obstet. 2022 Nov;159(2):365-371.
6. Gunderson CC, Nugent EK, Yunker AC, Rocconi RP, Graybill WS, Erickson BK, et al. Vaginal cancer: the experience from 2 large academic centers during a 15-year period. J Low Genit Tract Dis. 2013 Oct;17(4):409-13.
7. Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996 Jul;175(1):10-7.
8. Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD, Horner MJ et al. SEER Survival Monograph: Cancer Survival Among Adults: U.S. SEER Program 1988-2001, Patient and Tumor Characteristics. National Cancer Institute, SEER Program, NIH Pub. No. 07-6215, Bethesda, MD. 2007
9. Diagnosis, Therapy and Follow-Up Care of Vaginal Cancer and its Precursors. Guideline of the DGGG and OEGGG.
10. Karateke A, Tugrul S, Yakut Y, Gürbüz A, Cam C. Management of a case of primary vaginal cancer with irreducible massive uterine prolapse--a case report. Eur J Gynaecol Oncol. 2006;27(5):528-30.
11. Pardal C, Correia C, Serrano P. Carcinoma of the cervix complicating a genital prolapse. BMJ Case Rep. 2015 May 24;2015:bcr2015209580.
12. Bolovis DI, Brucker CVM. Non-obliterative modified LeFort colpocleisis with retained uterus. Annals of Gynecology and Obstetrics, in print.
Received: December 05, 2024;
Accepted: Janury 07, 2025;
Published: January 13, 2025.
To cite this article : Brucker CVM, Bolovis DI. Surgical Treatment For Locally Advanced Vaginal Cancer Associated With Total Utero-Vaginal Prolapse. British Journal of Cancer Research. 2025; 8(1): 736- 741. doi: 10.31488/bjcr.200.
© The Author(s) 2025. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/).
