Case Report / Open Access
DOI: 10.31488/bjcr.161
The Optimal Sequence of Adjuvant Treatments for Early-Stage Breast Cancer in the Partial Breast Irradiation Era: А Case Report
Míguez-Sánchez C*1, González-Ruiz MA1, Petrova D2, Ureña-Llinares A3, Gómez-Ruíz F1, Bayo-Lozano E1
1. Radiation Oncology Department, University Hospital Virgen Macarena, Seville, Spain
2. Andalusian School of Public Health, Granada, Spain
3. Medical Physics Department, University Hospital Virgen Macarena, Seville, Spain
*Corresponding author:Míguez-Sánchez C, Radiation Oncology Department, University Hospital Virgen Macarena, Seville, Spain
Abstract
Objective: Due to the implementation of new ultrashort radiotherapy schemes in patients with early-stage breast cancer, it is possible to propose a different sequence in adjuvant treatments. The objective of this work is to illustrate, through a clinical case, the feasibility of administering radiotherapy before systemic treatment without involving a substantial delay in it. Material and methods: We present the clinical case of a patient underwent to a right lumpectomy and SLNB. The pathological study revealed an infiltrating ductal carcinoma with medullary characteristics pT1c (2cm) pN0 (sn) M0, stage IA, grade 3, luminal B immunophenotype, with lymphatic, perineurial or vascular non-invasion and tumor-free resection margins. The sentinel node and periganglionic adipose tissue were negative. The MammaPrint genomic platform was requested and in the waiting time for results the patient received radiotherapy with an ultrashort regimen. Results: The patient was included in the observational study NCT04101656, currently in the recruitment phase. After surgical treatment, radiotherapy was performed on the surgical bed (APBI), total dose of 28 Gy / 5.6 Gy / fraction (5 sessions in 1 week). Acute and late skin toxicity was nil and the patient did not report any general symptoms. Conclusions: Patients with early-stage breast cancer should undergo radiotherapy as part of a conservative treatment with no clear evidence on the optimal sequence between radiotherapy and systemic treatment in terms of local control or overall survival. This case report shows that a different adjuvant treatment strategy is possible, performing radiotherapy immediately after surgery to complete local treatment, especially in patients who are going to undergo predictive genomic test. In these cases, thanks to ultrashort radiation therapy regimens, the starting of chemotherapy is not significantly delayed.
Keywords: Partial breast irradiation, early-stage breast cancer, sequence in adjuvant treatments
Background
The treatment of early-stage breast cancer is based on surgery, radiotherapy (RT), and systemic therapy (ST). Initially, the treatment of this pathology was very aggressive with maximum surgery, ablative chemotherapy (even rescue with hemopoietic precursors), and irradiation of all locoregional volumes (breast, axillary lymph nodes and internal mammary chain). That is, the maximum tolerable treatment was applied. This strategy was abandoned years ago, beginning a period of “de-escalation” with the aim of finding the most effective treatment with ST and locoregional RT (less is more) [1-4].
Regarding RT after conservative surgery, a total dose of 50 Gy has been traditionally performed in 25 fractions of 2 Gy / day, 5 days a week for 35 days [5,6]. However, other hypofractionated regimens have shown the same efficacy and are currently accepted as standard treatment. The most widely used regimens are those from the Canadian trial by Whelan [7] (42.5 Gy in 16 fractions of 2.66 Gy daily for 22 days) and the British trial START B (40 Gy in 15 fractions of 2.67 Gy, 5 days a week for 21 days).
More recently, the results of the United Kingdom study FAST FORWARD [9] demonstrated that 26 Gy in five fractions over 1 week is non-inferior to the START B trial regimen in terms of local control. Furthermore, adjuvant radiotherapy after surgery for early-stage breast cancer is well-tolerated and safe in terms of normal tissue effects up to 5 years.
Among the different hypofractionated schemes is the option of Accelerated Partial Breast Irradiation (APBI). For years, APBI has been considered a standard treatment in patients with good prognosis criteria [10,11]. Recently, the American Society of Radiation Oncology (ASTRO) [12], the American Society of Brachytherapy [13], and the American Society of Breast Surgeons [14] have updated these criteria, broadening the spectrum of candidate patients.
These recommendations are based on multiple studies showing long-term local control and overall survival results with APBI. For instance, the NSABP B-39/RTOG 0413 prospective randomized trial stands out for its design. It compares APBI, using 3D conformal external beam radiation therapy (3D-CRT), vs brachytherapy vs Whole Breast Irradiation (WBI). After 10 years follow-up, the results show an absolute difference of less than 1%, without statistical significance in the 10-year ipsilateral breast tumor recurrence-free interval (95.2% vs. 95.9%) between APBI and WBI [15]. Similarly, the RAPID randomized trial comparing APBI (3D-CRT 38.5 Gy / 10 fractions, twice daily) with WBI (42.5 Gy / 16 daily fractions or 50 Gy / 25 daily fractions ± tumor bed boost) has shown a local recurrence rate at 8 years of 3% vs 2.8% respectively, without statistically significant differences (HR = 1.27; 90% VI, 0.84-1.91) [16].
Recent studies have achieved similar results with treatment schemes more optimized for the operation of Radiation Oncology Departments, such as 30 Gy in 5 fractions on alternate days [17] or 27 Gy in 5 daily fractions of 5.4 Gy [18]. These regimens use external RT in short periods of time and can be applied in practically any modern Radiation Oncology Department with high precision and safety.
The future involves exploring different APBI fractionation schemes, including single-dose accelerated partial breast irradiation (S-APBI), already used in breast cancer before surgery or in breast cancer treated with only RT with radical intention. In these scenarios, S-APBI achieves good results in terms of local control and similar acute and late toxicities to longer RT regimens (even with concurrent chemotherapy) [19-21].
The increasingly widespread use of ultra - short fractionation schedules is laying the foundation for a new paradigm: the best sequence of adjuvant treatments after surgery in patients with early stage breast cancer.
Currently, treatment of initial stage breast cancer begins with conservative surgery followed by adjuvant treatment. The usual sequence is chemotherapy followed by radiotherapy when both are indicated. This sequence is a commonly accepted recommendation, with the aim of not delaying ST, although there is no clear evidence about which is the optimal sequence of both treatments [22].
However, ultra-short RT schemes, both APBI and FAST FORWARD, could modify the current sequence, allowing the administration of RT before ST. The purpose of this sequence is not to delay locoregional treatment, which in some cases can be administered after up to 6 months.
Objective
To demonstrate the feasibility of the proposed sequence, we present the clinical case of a patient, where ultrashort RT regimen was administered before ST in the treatment of early- stage breast cancer.
Case Report
A 53 year-old woman, asymptomatic, and without family history or personal background of interest. In screening mammography, an unpalpable tumor of 16 mm diameter with poorly defined edges and microcalcifications was visualized in the internal quadrants of the right breast (BIRADS 4c).
Complementary Tests
A breast ultrasound was performed with the same results as the mammography, including axillary exploration (no pathological nodes).The thick-needle biopsy (14/06/19) revealed an infiltrating ductal carcinoma, 100% estrogen receptors positive, 100% progesterone receptors positive, HER 2 negative (0%), Ki 67 90%, E-cadherin positive, CK19 positive, and p63 negative. Magnetic resonance imaging (MRI) results were: 15x16 mm neoplasm located in the internal quadrants of the right breast, located 25 mm from the areola-nipple complex and 60 mm from the posterior muscular plane. No other lesions suggestive of multifocality were observed. There were no significant findings in the left breast. Blood tests showed normal results including normal tumor markers: carcinoembryonic antigen0.88 ng / ml and CA 15.3 4.6 U / ml.
Treatment
The patient underwent right lumpectomy by SNOLL technique (Sentinel Node Occult Lesion Localization) and sentinel lymph node biopsy on 30/08/2019. The pathological study revealed an infiltrating ductal carcinoma with medullary characteristics pT1c(2cm)pN0(sn)M0, stage IA, grade 3, positive for receptors (100%), cERB-2 negative, Ki67: 90%, immunophenotype luminal B, no lymphatic, perineurial or vascular invasion, negative margins. Sentinel lymph node and adipose tissue near sentinel node were negative. The multidisciplinary committee decided to request MammaPrint genomic patform (16/10/19) to estimate the risk of local relapse and based on this result to apply ST. The patient was referred to the Radiation Oncology department for assessment.
Physical Examination
Patient with a good performance status (PS= 0). On right breast, depressed peri-areolar scar on the internal quadrants with second intention signs of scarring. Axillary scar well healed with normal aspect. No lymphatic stasis or inflammatory signs on the right breast. No pathological findings in the left breast.
While the patient was waiting for results from the genetic platform, it was decided on the breast cancer committee to perform adjuvant RT before ST. The proposed RT scheme was APBI because of clinical criteria. The patient was included in the observational study FIS- APBI-2019-02, currently in its recruitment phase. She underwent radiotherapy on the surgical bed of the right breast + margins (according to protocol), total dose of 28 Gy, with a fractionation of 5.6 Gy / fraction between 29/10/19 and 05/11/19.

Figure 1:Patient photograph before radiotherapy (A) and 1 year after radiotherapy (B). Note that the right breast size is at a smaller than the left breast, after surgery and previous radiotherapy. The right breast size and colour are the same before and after radiotherapy.
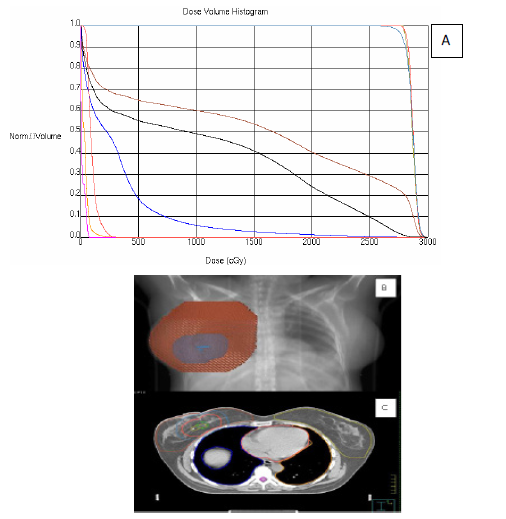
Figure 2:A. Dose-volume histogram (DVH) from patient treatment plan. B. Portal image and digitally reconstructed radiograph (DRR) C. CT with target volume and organ at risk. Ipsilateral breast Ipsilateral breast without PTV Right lung Left lung Heart Spinal cord Surgical bed CTV PTV
The tumor volumes of treatment were the clinical tumor volume (CTV) and the planning tumor volume (PTV). The CTV consists of the surgical bed, marked with metal clips during the surgery plus a homogeneous expansion in all directions of 1.5 cm. The CTV cannot exceed the limits of the breast. The PTV is CTV plus 1 cm margin in all directions. The treatment was conducted with 6 MV photons and intensity modulated radiotherapy technique (IMRT). Prior to the administration of RT, daily image controls were performed to ensure its accuracy (IGRT).
On 30/10/19, the genomic platform revealed high risk of local relapse results and the patient started four cycles of adjuvant chemotherapy (adriamycin and cyclophosphamide regimen) from 13/11/19 to 29/01/20. Subsequently, she started hormonal therapy with tamoxifen 20 mg / day, which is still ongoing.
Follow-up
At the end of the treatment, acute skin toxicity was nil and the patient did not report any general symptoms. Follow-up appointments took place one week, one month, 6 months, and 1 year post-treatment. The patient continues to be asymptomatic, without acute or late toxicity related to RT on examination.
Discussion
Patients with early-stage breast cancer should undergo RT as part of conservative treatment with no clear evidence on the optimal sequence between RT and ST in terms of local control or overall survival. This case report shows that a different adjuvant treatment strategy is possible, performing RT immediately after surgery in order to complete local treatment, as occurs, for example, with intraoperative radiotherapy (IOR) [23].
On one hand, it has been demonstrated that the delay between conservative surgery and RT is related to a higher probability of local recurrence, with a relative risk of local recurrence per month of delay of 1.08 (1.02-1.14) [24]. On the other hand, a randomized study of 244 patients showed that delaying ST after RT can increase the rate of distant metastases. However, this study also showed that delaying RT after ST leads to an increased risk of local recurrence (5% RT-CT versus 14% CT-RT) [25] .
This controversy could be resolved with the synchronous performance of both treatments (RT and ST). Recently, a study conducted in 48 UK hospitals (SECRAB study) tested this possibility and showed that synchronous chemo-radiotherapy significantly improved local recurrence rates with an acceptable increase in acute toxicity [26].
Currently, thanks to new RT dose and fractionation regimens (APBI in 5 sessions in 1 week duration [18] or ultra-short hypofractionation on the whole breast [9]), it is possible that patients with early stage breast cancer can receive RT immediately after surgery without significantly delaying the start of chemotherapy. Additionally, a significant percentage of these patients are candidates for genomic tests that help to establish the best ST strategy [27]. The waiting period for the test results would facilitate the performance of the different ultra-short hypofractionated schedules of RT without an additional delay in starting chemotherapy.
In our opinion, and according to our practice at the Virgen Macarena University Hospital, success lies in a multidisciplinary approach between medical and radiation therapy oncologists who jointly decide on the optimal sequence of adjuvant treatments, considering the possibility of performing ultra-short RT schemes (APBI or WBI in 1 week), especially in patients who are going to undergo predictive genomic tests. This way, it would be possible not to delay RT until the end of ST, as can be seen in the clinical case that we have presented. Finally, the S-APBI scheme, preoperatively or adjuvant, may be the standard definitive step to first complete local treatments (surgery and RT) and then perform ST.
Conclusions
Patients with early breast cancer should undergo RT as part of their adjuvant treatment, with no clear evidence on the optimal sequence between RT and ST. The performance of RT with ultrashort hypofractionated regimens immediately after surgery and prior to ST is feasible. This sequence could become the standard strategy of adjuvant treatment in patients waiting for results of genomic tests.
References
1. Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002; 347(16):1227-32.
2. Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Lancet. 2005;366(9503):2087-106.
3. Winchester DJ, Menck HR, Winchester DP. The national cancer data base report on the results of a large nonrandomized comparison of breast preservation and modified radical mastectomy. Cancer. 1997; 80:162-7.
4. Morris AD, Morris RD, Wilson JF, et al. Breast-conserving therapy vs mastectomy in early stage breast cancer: a meta-analysis of 10-years survival. Cancer J Sci Am. 1997; 3:6- 12.
5. Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347(16):1233-41.
6. Van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000; 92(14):1143-50.
7. Whelan T, MacKenzie R, Julian J, et al. Randomized trial of breast irradiation schedules after lumpectomy for women with lymph node-negative breast cancer. J Natl Cancer Inst . 2002; 1143-1150.
8. START Trialists' Group, Bentzen SM, Agrawal RK, et al. The UK Standardisation of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet. 2008;371(9618):1098-107.
9. Brunt, AM, Haviland, JS, Wheatley DA, et al, on behalf of the FAST-Forward Trialists. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST- Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non- inferiority, randomised, phase 3 trial. Lancet.2020.
10. Correa C, Harris E, Leonardi MC, et al. Accelerated Partial Breast Irradiation: Executive summary for the update of an ASTRO Evidence-Based Consensus Statement. Practical Radiation Oncol. 2017; 7: 73-79.
11. Polgár C, Van Limbergen E, Pötter R, et al. GEC-ESTRO breast cancer working group. Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: recommendations of the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group based on clinical evidence (2009). Radio ther Oncol.2010;94(3):26473.
12. Correa C. Accelerated Partial Breast Irradiation: Executive summary for the update of an ASTRO Evidence-Based Consensus Statement. Practical Radiation Oncol. 2017; 7:73-79.
13. The American Brachytherapy Society consensus statement for accelerated partial-breast irradiation. Brachyther. 2018;17: 154 - 170.
14. The American Society of Breast Surgeons. Consensus Guideline on Accelerated Partial Breast Irradiation. 2018.
15. Vicini F, Cecchini R, White J, et al. Long-term primary results of accelerated partial breast irradiation after breast-conserving surgery for early-stage breast cancer: a randomised, phase 3, equivalence trial. Lancet. 2019; 394: 2155–64.
16. Whelan T, Julian J, Levine M, et al. RAPID: A randomized trial of accelerated partial breast irradiation using 3-dimensional conformal radiotherapy (3D- CRT). https://www.abstracts2view.com/sabcs18/view.php?nu=SABCS18L_1220. Published (2018).
17. Livi L, Meattini I, Marrazzo L. Accelerated partial breast irradiation using intensity- modulated radiotherapy versus whole breast irradiation: 5-year survival analysis of a phase 3 randomized controlled trial. Eur J Cancer. 2015; 51:451-463.
18. Grendarova P, Roumeliotis M, Quirk S. One-Year Cosmesis and Fibrosis From ACCEL: Accelerated Partial Breast Irradiation (APBI) Using 27 Gy in 5 Daily Fractions. Practical Radiation Oncol.2019); 9: e457-e464.
19. Bondiau P, Courdi A, Bahadoran P. Phase 1 clinical trial of stereotactic body radiation therapy concomitant with neoadjuvant chemotherapy for breast cancer. Int J Radiat Oncol Biol Phys. 2013; 85(5):1193-1199.
20. Palta M, Yoo S, Adamson J. Preoperative single fraction partial breast radiotherapy for early-stage breast cancer. Int J Radiat Oncol Biol. 2012; 82 (1): 37-42.
21. Blitzblau R, Arya R, Yoo S. A phase 1 trial of preoperative partial breast radiation therapy: Patient selection, target delineation, and dose delivery. Pract Radiat Oncol. 2015; 5:e513- e520.
22. Hickey BE, Francis DP, Lehman M. Sequencing of chemotherapy and radiotherapy for early breast cancer. Cochrane Database of Systematic Review. 2013; 4. Art. No.: CD005212.
23. Vaidya J, Bulsara M, Baum M, et al. Long term survival and local control outcomes from single dose targeted intraoperative radiotherapy during lumpectomy (TARGIT-IORT) for early breast cancer: TARGIT-A randomised clinical trial. BMJ. 2020;370:m2836.
24. Gupta S, King W, Korzeniowski et al. The Effect of Waiting Times for Postoperative Radiotherapy on Outcomes for Women Receiving Partial Mastectomy for Breast Cancer: a Systematic Review and Meta-Analysis. Clin Oncol (R Coll Radiol). 2016; 28(12):739-749.
25. Recht A, Come SE, Gelman RS, et al. Integration of conservative surgery, radiotherapy, and chemotherapy for the treatment of early-stage, node-positive breast cancer: sequencing, timing, and outcome. J Clin Oncol.1991;9(9): 1662e1667.
26. Fernando IN, Bowden SJ, Herring K, et al. Synchronous versus sequential chemo- radiotherapy in patients with early stage breast cancer (SECRAB): a randomised, phase III, trial. Radiother Oncol. 2020;142:52-61.
27. Nicolini A, Ferrari P, Duffy M. Prognostic and predictive biomarkers in breast cancer: Past, present and future. Semin Cancer Biol. 2018;52(Pt 1):56-73.
Received: January 04, 2021.
Accepted: February 23, 2021
Published: February 25, 2021.
To cite this article : Míguez-Sánchez C, González-Ruiz MA, Petrova D, et al. Altered Transcriptome in Pediatric AML Compared with Normal Hematopoiesis. British Journal of Cancer Research. 2021; 4:1.
©2021 Míguez-Sánchez C, et al. .
