Research article / Open Access
DOI: 10.31488/bjcr.192
The Perception of Pain in the Experience of Childhood Cancer
Hilze Benigno de Oliveira Moura Siqueira1, Amanda Batista Vilarindo2, Rodrigo Ramon Falconi Gomez3, Simone Saltareli4, Talita de Cassia Raminelli da Silva3, Fátima Aparecida Emm Faleiros Sousa2
1. Estácio IDOMED, Juazeiro-BA, Brazil
2. University of São Paulo, Brazil
3. Euro-American University Center, UNIEURO, Brazil
4. Paulista University, UNIP, Ribeirão Preto - SP, Brazil
*Corresponding author:Fátima Aparecida Emm Faleiros Sousa, Full Professor, Clinical Psychophysics Laboratory, University of São Paulo at Ribeirão Preto, Brazil.
Abstract
There is interest in pediatric cancer pain and its assessment, but it is less studied about scientific production in adults. The study aimed to evaluate how children/adolescents with cancer and family caregivers understood pain. The following instruments were used: sociodemographic and clinical indicators of pain and illness, the Faces Affective Scale (FAS), and the Multidimensional Pain Assessment Scale (EMADOR). Results: age distribution (05-07, 08-11 and 12-19 years old), prevalence for 12-19 years old (45%), female sex (53%), incomplete elementary school (95%) and Catholics (62%). Higher rates for chronic pain (51%) and leukemia (47%). In FAS, figures representing variation in the negative effect of pain were most indicated (71%). In EMADOR, the results by age group showed the descriptors characterized in acute pain about the affective and cognitive dimensions; however, the perception of chronic pain was understood following the life cycle reasoning, from concreteness in sensory descriptors to abstract understanding in affective descriptors. It was concluded that pain was thought of multidimensionally. EMADOR was considered an easy and reliable instrument for pain assessment in the development process, children from the age of 5 understood the painful phenomenon, and mothers, after their children, are the ones who most understand their pain, bringing possibilities for better management of the phenomenon.
Keywords: Pain, cancer, child, adolescent, famíly, development
Introduction
Childhood cancer in the last four decades has shown a significant increase in the incidence of new cases. It is estimated that 430 thousand new cases of cancer occur in Brazil, in children and adolescents aged 0 to 19 years. Childhood cancer, although considered rare when compared to the adult population, is the second cause of child and youth mortality in the 0 to 19-year-old age group in the country. Worldwide, this is the main cause of mortality in children over 1 year of age. The main treatment chosen for most cases is chemotherapy, but there is the possibility, depending on the case, of surgery, radiotherapy, and transplants [1,2].
The fear of cancer is evident due to the possibility of pain throughout the disease process, from the moment of diagnosis to the uncertainties arising from this moment to be faced. Several aspects need to be considered in this scenario, including the treatment approach, psychosocial aspects of the individual and family, pain management and symptoms associated with the disease, as well as acceptance of the diagnosis [2].
Among the feelings and behaviors that can affect a child during hospitalization when faced with a cancer diagnosis is the phenomenon of pain. The diagnosis, the uncertainties, the emotions that manifest themselves, and the impact on the routine have repercussions on the entire family, which can even lead to the emergence of disorders that affect the child's development [3,4]. It is understood that pain is perceived according to the concept of total pain.
Assessing the perception of pain in cancer and its multidimensionality represents an immense challenge, as it is not enough to just know the etiology of pain, it is necessary to be aware of human suffering based on the perception and expression of those who experience the painful experience [5]. At this core, many questions may arise, such as, for example, how does the child think and perceive this experience? What type of pain do you express and how do you understand that pain? How does the family perceive the pain of a loved one with cancer?
It is worth mentioning that pain assessment measures correspond to both self-report and behavioral observations, as well as physiological measures, such as heart rate and blood pressure; these are considered complementary measures to the first. Among pain indicators, variables such as cognition, emotion, motivation, among others from the environmental context can influence the perception, intensity, sensation, and quality of the pain experience stand out. In this sense, in the field of measuring pain attributes, when only sensory characteristics of this phenomenon are considered (intensity, for example), its other dimensions are nullified and, consequently, the problem of pain is not perceived in its entirety [6,7].
Because pain is a complex phenomenon, multidimensional scaling constitutes a set of tools capable of capturing the pain experience that varies in intensity throughout the integration of multiple factors, such as sensory, affective, behavioral attributes, and cognitive correlates. Several studies have validated and used these scales as a means of understanding the different dimensions associated with pain and clinical situations. One example is the Multidimensional Pain Assessment Scale, also known as EMADOR [5,8-10].
Therefore, the use of unidimensional and multidimensional instruments is essential for a better understanding of the universe that involves the measurement of pain. However, first of all, it is necessary to qualitatively listen to others with empathy, interest, and respect for differences and subjectivity, and the meaning of experience without inferences from values and beliefs so that perception is not distorted [11,12].
The nature of human perception has long been of interest to several areas of knowledge. There is nothing more important than knowing your own experiences and those of other people, as this is a complex process capable of influencing how each person understands their experiences of joy, satisfaction, sadness, or pain. When it comes to understanding events, we think of “perception” and “experience” [13].
Psychophysics and its methodological rigor are scientifically recognized, based on Stevens [14], which postulates measurement criteria with the possibility of being expressed at four scalar levels: nominal, ordinal, interval, and ratio. Nominals are used to name, identify and/or categorize (pain versus non-pain); ordinals, order the object of study according to certain comparison characteristics (non-pain, mild pain, moderate pain and strong pain); interval ones, have fixed intervals between numbers and allow comparing differences between measurements, being a relative measurement (pain thermometer expressed in centimeters); and those of ratio, in which there is an absolute zero and, therefore, allows us to conclude regarding the absolute magnitude of the measurement in question [12,15].
To identify and/or categorize pain, one of the psychophysical methods used is category estimation, in which subjects estimate their experiences through structured scales with clear limits. Such scales, being simple, assess pain using verbal or visual descriptors [5,14].
Therefore, this study aimed to evaluate the perception of pain in the experience of childhood cancer, in addition to understanding how family members (caregivers) perceive the painful experience in this context.
Method
Study design
Descriptive exploratory study based on human development from the perspective of the life cycle and psychophysics.
Place and Period
The investigation was carried out at the Hospital das Clínicas of the Faculty of Medicine of Ribeirão Preto of the University of São Paulo, specifically, in the outpatient clinic and in the pediatric oncology ward of the Department of Childcare and Pediatrics of that institution. Data collection was carried out from March 2010 to June 2012, with the protocols developed in a maximum time of 1h30min.
Participants
Children and adolescents participated in the study, with their accompanying family members. The selection of these participants followed the inclusion criteria: ages between 5 and 18 years old, of both sexes, with the condition of undergoing cancer treatment, regardless of the stage of the treatment and the type of neoplasia. Those who did not have sufficient physical and understanding conditions to perform the tasks requested in the research were excluded. For companions, the only selection criterion was being a family member who was with the child/adolescent in the role of caregiver.
Ethical aspects
Based on Resolution 196/96 on research with human beings, this investigation was approved by the Research Ethics Committee of the Faculty of Medicine (Crafts - Process no. 3926/2009) and linked to the service that served as the setting for this study. It is important to highlight that the Terms of Informed Consent (TCLE) and Free and Informed Assent (TALE) were applied. Furthermore, the names of the participating children/adolescents were changed and identified with code names alluding to precious stones, to guarantee their anonymity. It is important to highlight that the choice to change the participants' names to names of precious stones arose from the similarity between the painful stages of childhood cancer (diagnosis, treatment, coping and adaptation) and the stages of cutting precious stones (cutting , pre-training, training and polishing) and also because we understand the preciousness of the lives of these children/adolescents with cancer.
Procedure
First, a pilot test was carried out for all data collection instruments, for which 15 children/adolescents from each age group between 5 and 19 years old were selected for convenience. Then, the instruments were applied, after consulting medical records to identify the study participants and better understand the characterization of pain and disease.
Therefore, the instruments and procedures established during the data collection process will be presented below:
1. Questionnaire on socio-demographic indicators and characterization of pain and disease: This questionnaire was designed and applied to collect data, such as age, sex, level of education, religion and city of origin of the participants. Added to these, too clinical data on the disease were researched, such as time since diagnosis/treatment and phase of the disease; in addition to other data on acute and/or chronic pain.
2. Emotional Faces Scale: Validated in the revised version by McGrath et al. [16-18] is composed of nine different facial expressions, ordered sequentially by the letter range (A-I) and by the neutral point of the scale (E), which measures from 'absence of pain' to 'highest degree pain', making it possible to investigate the meanings of positive (A, B, C, D) and negative (F, G, H, I) effects of pain. In this way, participants chose among the nine faces, ordered on a scale from A to I, as mentioned previously, the one that most indicated the intensity of pain perceived.
3. Multidimensional Pain Scale (EMADOR): Validated by Faleiros et al. [5] for Portuguese-speaking culture, this instrument can be applied to the most diverse experiences and stages of human development. Consisting of 50 descriptors and respective meanings, characterized by acute and chronic pain, whose response alternatives are eleven points graded from zero (0) to ten (10), which depending on the score that is paired with each descriptor makes it possible to capture the sensory dimensions, affective and cognitive pain. Data were analyzed using the Statistical Package for the Social Program Sciences (SPSS) version 19.0 for Windows based on data extracted from each instrument used.
Materials
The following were used: a recorder, K-7 tapes, pencil, and graphic materials (paper sheet containing EMADOR scale).
Results
Regarding the pilot test stage, there were no suggestions for changes despite the items in the different instruments. The information obtained through sociodemographic data shows a slight predominance of females (53.0%) over males (47.0%). Regarding the age variable, the results were organized into three age groups (05-07, 08-11 and 12-18 years old), with the most prevalent group being the 12 to 18-year-old age group, covering a percentage of 45%. of the participants. our results showed the level of education, with the majority of representation (95.0%). Concerning the city of origin or origin of the children/adolescents, the city in the Ribeirão Preto Region received greater prominence (42%), followed by other states in the country (30%) represented by Sergipe, Bahia, Mato Grosso do Sul, Distrito Federal, Minas Gerais among others.
In the “religion” attribute, more than half of the participants (62.0%) described belonging to the Catholic religion, in addition to the evangelical religion (24.0%), the spiritualist religion (2.0%) and some expressed not having any type of belief. religious (11.0%).
Regarding childhood cancer indicators, the data showed the percentage distribution of neoplasms, as seen in Figure 1.
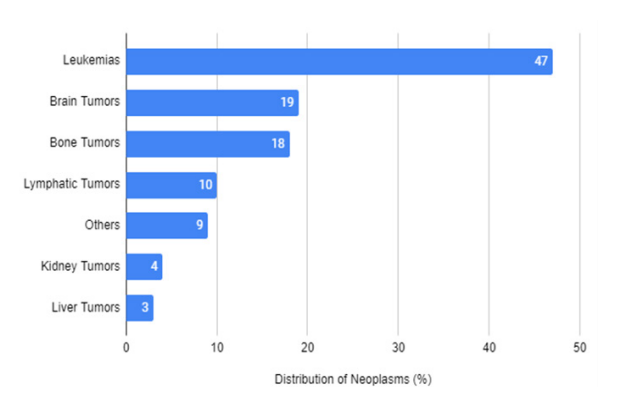
Figure 1:Percentage distribution of pediatric neoplasms in the investigated sample (n=100)
Regarding the general average time between diagnosis and treatment, an average of 01 years and 04 months was observed for evaluation and technical procedures of the disease. Each treatment (management) of the disease experienced by the children and adolescents in this study can be seen in Table 1.
Table 1. Childhood cancer therapies with percentage by number of study participants (n=100).
| Disease Therapeutics | % |
|---|---|
| Chemotherapy | 46 |
| Radiotherapy | - |
| Surgery | 08 |
| Chemotherapy + Surgery | 12 |
| Chemotherapy + Radiotherapy | 06 |
| Chemotherapy + Radiotherapy + Surgery | 14 |
| Control Phase | 14 |
Regarding the characterization of the types of chronic and acute pain, it was observed that both was no significant difference between the results, with the percentage distribution for complaints of chronic pain (≥ 3 months) of 51% and acute pain (≤ 3 months). ) of 49%.
The temporality of pain was investigated in our study, encompassing the period before management and the present moment of the interview. The past of pain was mentioned by 97% of our participants and their pain responses were linked to physical, emotional and social experiences. On the other hand, complaints of pain at the time of the interview were described by 18% of children/adolescents with cancer. Those who did not want to report on the phenomenon were around 6%.
Overall, it is interesting to mention that children/adolescents thought and answered the question regarding pain time through the perception of the physical, situational and affective dimensions of pain, as shown in Table 2.
Table 2. Pain perception and response to pain time related to thechild's experience and teenagers with cancer.
| Pain Perception | Response to the temporal experience of pain |
| Physical pain | Pain complaints in parts of the body such as: head, legs, back, entire body, throat, abdomen, stomach, foot, back of the neck. |
| Contextual | Painful experiences in the social context (family problems, loss of school and friends) and in the therapeutic clinical context (therapeutic procedures in the hospital, length of stay in hospital). |
| Affective | Longing, fear of bullying. |
McGrath's Affective Face Scale (FAS) [16-18] was analyzed, observing the choice of nine sequential faces, referring to the reality of each participant's pain. Then, the perception of pain was considered by the scalar variation of positive effect (A-D: no pain), negative effect (F-I: different degrees of painful intensity), the neutral point of the scale (face E) and respective meanings. The results were presented through the general percentage distribution of the scalar amplitude demonstrated by the faces chosen by the sample participants, as shown in Table 3.
Table 3. Analysis of McGrath's Revised Visual Scale [17], corresponding to perceptions regarding the positive and negative effects of pain in the percentage distribution of research participants (n=100).
| Range of variations of positive and negative effects in relation to pain | Overall percentage distribution |
|---|---|
| A - D | 13% |
| E | 16% |
| F - I | 71% |
In general, Table 3 shows the variations related to negative effects, represented by faces F–I, whose percentage distribution was 71%, according to the attributions of the children/adolescents researched, with 28% being indicated for face F, 19% for face G, 8% and 16% for faces H and I, respectively.
The faces represented A–D were highlighted by 13% of the participants, with the majority (8%) choosing face D. Regarding the application of EMADOR, it was possible to observe that, of the 100 children/adolescents with cancer investigated, 29% attributed meanings to some descriptors, even before knowing the formal contextual meaning belonging to the instrument and 71% responded to the descriptors after explanations, but without attributing their meanings to the descriptors. These results can be seen in the Table below, which shows the distribution by age group represented by children aged 5-7 and 8-11, as well as teenagers aged 12-18.
We chose to analyze EMADOR using the psychophysical Category Estimation method. Thus, the Arithmetic Mean (AM), Standard Deviation (SD) and Standard Error of the Mean (SEM) were calculated. Next, the descriptors that obtained the highest and lowest attribution in the characterization of acute or chronic pain were observed. Finally, they were organized into tables and graphs, descriptively.
Regarding the analysis of the 100 participating children/adolescents, 51% reported chronic pain and 49% acute pain. It is important to clarify that 105 children were selected, however, five were excluded from the study; three, because they were unable to understand the words that described the pain, chose not to complete the task and two did not want to participate due to the same situation, that is, the need to leave the research site due to the public transport schedule to the city of origin.
Table 3. Analysis of McGrath's Revised Visual Scale [17], corresponding to perceptions regarding the positive and negative effects of pain in the percentage distribution of research participants (n=100).
| Range of variations of positive and negative effects in relation to pain | Overall percentage distribution |
|---|---|
| A - D | 13% |
| E | 16% |
| F - I | 71% |
Among EMADOR's chronic pain descriptors, the most highlighted by children/adolescents were 'unpleasant' (7.78±2.60), 'boring' (7.67±2.73), 'painful'(7, 29±3.06), 'uncomfortable'(7.18±2.62) and 'exhausting'(7.04±3.28), revealing a significant score in the characterization of chronic pediatric cancer pain. On the other hand, the descriptors with the lowest attribution were 'overwhelming' (4.21±3.33), 'disastrous' (4.86±3.36), 'devastating' (4.90±3.72), ' burning'(5.00±4.00) and 'suffocating'(5.06±3.38).
Table 4. Distribution of descriptors contained in EMADOR with some meanings attributed by children/adolescents, according to age group.
| Age Range | Chronic Pain Descriptors | |
|---|---|---|
| Infernizing | “It bothers other people” (Lapis Lazuli, 05 years old) | |
| Miserable | “Evil” (Lapis-lazúli, 05 years) | |
| Depressing | “That makes me very sad” (Chinese lyrics, 07 years); “Just as I feel very sad” (Precious Jasper, 5 years old) | |
| Painful | “Painful in the leg” (Green Gold, 07 years old) | |
| Unbearable | “Unbearable in the head” (Green Gold, 07 years old) | |
| Scary | “Don’t let me study” (Green Gold, 07 years old) | |
| Maddening | “Go crazy” (Green Gold, 7 years old) | |
| Punitive | “Just like punishment” (Green Gold, 07 years old) | |
| Burning | “That burns” (Precious Jasper, 05 years old) | |
| Torturous | “Bad as the big bad wolf ” (Green Gold, | |
| 07 years) | ||
| Acute Pain Descriptors | “That’s not right in the head” (Rose Quartz, 07 years old) | |
| Burglar | “That steals from us” (Rose Quartz, 07 years old) | |
| Aggressive | “What’s fighting with us?” (Rose Quartz, 07 years old) | |
| Colossal | “Is it a bone? A big bone?” (Rose Quartz, 07 years) | |
| Like a stab | “That hits hard” (Rose Quartz, 07 years old) | |
| Like shock | “Like shock in the socket?” (Epidote, 7 years old) | |
| Distressing | “It makes your heart sink” (Esmeralda, 6 years old) | |
| Clear | “Like the sun, what do I see?” (Esmeralda, 6 years old) | |
| How Needled | “Like an injection needle” (Esmeralda, 06 years old) “Like a knife that cuts” (Esmeralda, 06 years old); | |
| Cutting | “Like a saw” (Berilo, 5 years old) | |
| Fiery | “Like pepper” (Berilo, 5 years old) | |
| Discouraging | “No desire” (Berilo, 05 years old). “That you don’t want to continue?” (Esmeralda, 6 years old). | |
Regarding the EMADOR acute pain descriptors, the most attributed by children/adolescents with cancer were “boring” (cognitive), “unpleasant” (affective), “painful” (sensitive), “uncomfortable” (sensitive) and “clear ”(sensitive), which implies an understanding of pain more focused on the sensitive dimension, although there are cognitive and affective elements involved in this understanding. About the descriptors that were categorized with lesser attributions, the highlights are “overwhelming” (affective), “cold” (sensitive), “cutting” (sensitive), “like shock” (sensitive), and “desperate” (affective). This demonstrates that the cognitive dimension was not represented in the descriptors relating to the lower attribution of acute pain in the experience of childhood cancer.
When we went through our study, we realized that the importance of using a multidimensional assessment instrument was considered when EMADOR was applied to children/adolescents at different stages of cancer and development, due to this, we found the need to present how the distribution was of pain qualification by chronic and acute characterization descriptors, according to the age groups researched. Therefore, these data were presented as shown in Table 5.
Table 5. Characterization of EMADOR (chronic pain and acute pain) in relation to age group.
| Age Range | Descriptors | AM | SD | SEM | Descriptors | AM | SD | SEM |
|---|---|---|---|---|---|---|---|---|
| 05-07 years | Biggest assignment | Biggest assignment | ||||||
| Painful | 7,54 | 2,47 | 0,68 | Complicated | 8,20 | 2,34 | 0,74 | |
| Terrifying | 7,08 | 3,06 | 0,85 | Boring | 8,00 | 2,86 | 0,90 | |
| Strong | 6,92 | 3,94 | 1,09 | Unpleasan | 7,80 | 2,39 | 0,75 | |
| Excessive | 6,85 | 3,82 | 1,06 | Slashing | 7,70 | 3,33 | 1,05 | |
| Boring | 6,77 | 2,42 | 0,67 | Unbridled | 7,30 | 3,12 | 0,98 | |
| Minor assignment | Minor assignment | |||||||
| Disastrous | 3,31 | 3,61 | 1,00 | Scary | 2,80 | 2,04 | 0,64 | |
| Devastating | 3,92 | 3,49 | 0,97 | Circular | 2,90 | 3,24 | 1,02 | |
| That spreads | 4,69 | 3,79 | 1,05 | Cutting | 3,10 | 3,84 | 1,21 | |
| Harmful | 4,85 | 3,26 | 0,90 | Mad | 3,80 | 3,79 | 1,20 | |
| Scary | 5,00 | 3,95 | 1,09 | Deliberative | 3,90 | 2,80 | 0,88 | |
| 08-11 years | Biggest assignment | Biggest assignment | ||||||
| Cursed | 7,40 | 3,58 | 0,92 | Unpleasant | 6,94 | 3,47 | 0,86 | |
| Unpleasant | 7,33 | 2,79 | 0,72 | Painful | 6,81 | 2,92 | 0,73 | |
| Boring | 7,20 | 3,18 | 0,82 | Boring | 6,63 | 3,09 | 0,77 | |
| Strong | 7,13 | 3,96 | 1,02 | Considerable | 6,00 | 3,55 | 0,88 | |
| Unbearable | 6,93 | 3,51 | 0,90 | Uncomfortable | 5,81 | 2,88 | 0,72 | |
| Minor assignment | Minor assignment | |||||||
| Overwhelming | 3,06 | 3,45 | 0,89 | Overwhelming | 1,38 | 2,65 | 0,66 | |
| Persistent | 3,60 | 2,77 | 0,71 | Cold | 1,69 | 2,21 | 0,55 | |
| Suffocating | 3,80 | 3,93 | 1,01 | Desperate | 2,13 | 2,44 | 0,61 | |
| Depressing | 4,20 | 2,80 | 0,72 | Like shock | 2,25 | 3,04 | 0,76 | |
| Distressful | 4,53 | 2,85 | 0,73 | Mad | 2,38 | 3,09 | 0,77 | |
| 12-18 years | Biggest assignment | Biggest assignment | ||||||
| Boring | 8,48 | 2,46 | 0,51 | Boring | 7,57 | 2,88 | 0,60 | |
| Unpleasant | 8,22 | 2,17 | 0,45 | Unpleasant | 7,13 | 2,45 | 0,51 | |
| Uncomfortable | 8,17 | 1,77 | 0,37 | Uncomfortable | 5,96 | 3,25 | 0,67 | |
| Bother | 8,13 | 2,30 | 0,48 | Clear | 5,91 | 3,89 | 0,81 | |
| Queasy | 7,96 | 4,42 | 0,50 | Burglar | 5,98 | 3,25 | 0,67 | |
| Minor assignment | Minor assignment | |||||||
| Continuous | 4,87 | 2,75 | 0,57 | Cutting | 2,57 | 3,40 | 0,71 | |
| Devastating | 4,91 | 3,65 | 0,76 | Cold | 2,70 | 3,41 | 0.71 | |
| Burning | 4,96 | 3,66 | 0,76 | Desperate | 2,74 | 3,07 | 0,64 | |
| That spreads | 5,04 | 3,84 | 0,80 | Crazy | 3,13 | 4,05 | 0,84 | |
| Overwhelming | 5,13 | 2,68 | 0,55 | Destroyer | 3,17 | 3,40 | 0,71 |
AM = Arithmetic Mean
SD = Standard Deviation
SEM = Standard Error of the Mean
Discussion
In some studies on pediatric cancer, we observed that age groups vary significantly. This variation had in its sample participants aged 3 to 12 years [19] and 7 to 12 years [20]. According to INCA [21], it is estimated that between 70% and 80% of children diagnosed early with neoplasms can be cured. In addition to the objective of disease remission, there is also a focus on minimizing the discomfort arising from this clinical condition.
The literature points out that new scientific technologies have opened up ways to carry out early diagnosis, in shorter periods, to provide a better quality prognosis for the person and an improvement rate of the disease [22]. A study that worked on cancer prevention and health promotion for the 21st century, “advances in recent decades have been evident, but equity in health promotion and cancer prevention has not yet been achieved”. Public policies need to consider society, its culture, socioeconomic aspects and proactive behaviors [23].
The survival rates already presented relate to a diverse range of factors, such as sex and age, location, extension, and type of tumor. Furthermore, for a favorable prognosis, care for children and adolescents must take place in health services dedicated to the specialty, with properly trained teams.
Even considering the gradual increase in the number of children with cancer as pointed out by some studies [21,24], it is also possible to observe progress in therapies aimed at childhood neoplasms, the most common of which are: leukemias, central nervous system tumors, and lymphomas. These data corroborate those of the present investigation as shown in Figure 1.
About the pain phenomenon, other studies on cancer, despite not having the objective of working specifically with the pain phenomenon, can show organic and psychosocial aspects that refer to pain in children and/or adolescents, through events in the child's life or of the adolescent resulting from the disease, as a grieving process and meaning of death; the meaning of being in the hospital; child suffering, changes in self-image, shame about their physical appearance, feelings of anger over lost friendships, denial of reality and passive acceptance of the therapeutic modalities applied to them [25-28].
In this sense, a carried out a study to evaluate the psychosocial impacts and quality of life in children and adolescents with cancer. It was a cross-sectional, descriptive study. The method consisted of applying PedsQL 4.0 - Quality of Life and PedsQL 3.0 - Cancer Module. The results presented were 25 pediatric oncology patients between 8 and 18 years old (group 8-12 years old and group 13-18 years old). A significant impact on quality of life was identified. In the Quality of Life module, the groups did not show a significant difference (p=0.627) between the groups of patients, however in the Cancer Module (p=0.0094) the group aged 8 to 12 years had a significantly greater impact. We tend to attribute that a potentially important variable to explain this difference is the fact that the groups are at different stages of the life cycle. It is worth noting that the study showed that younger people suffered a greater psychosocial impact. This impact is described by fear, sadness, and anger, linked to hospitalization and changes in routine. Negative feelings were also associated and heightened with invasive procedures. The descriptors “I feel afraid” and “I feel pain” were present and when asked about physical pain, the impacts described by the participants were pain and getting hurt in the “joints” and muscles [29].
In an investigation to evaluate the symptoms of adolescents with cancer admitted to a Pediatric Oncology Service for chemotherapy treatment. This investigation was characterized as multi-method research. Regarding the sample, there were 10 adolescents diagnosed with cancer and hospitalized to undergo the chemotherapy procedure from August 2019 to March 2020. The adolescents were evaluated three consecutive times during two cycles of chemotherapy, using the SSPedi scale. BR and complementary instrument for symptom assessment. To analyze these data, we opted for cross-synthesis of the data with the help of the R Core Team program for statistical analyses. The results indicate that adolescents aged between 11 and 18 years demonstrated the most frequent symptoms: nausea and vomiting (average score = 1.75), lack of appetite (1.73), changes in taste (1.22), tiredness (1.07), and mood changes (0.52). In combination with data from the complementary questionnaire, the symptoms: of nausea, vomiting, pain, and dry lips were indicated as the most frequent [30].
Pain is reported in a wide proportion of adult patients hospitalized for cancer treatment, ranging from 58% to 80%. In children, the prevalence of pain is notable, with an incidence of 78% during diagnosis, between 25% and 58% throughout treatment, and reaching up to 90% in the terminal phase of the disease. We understand that all the questions mentioned above brought, even if implicitly, content related to pain in its various dimensions. They are identifiable by the characteristics of the clinical condition such as nausea and vomiting, lack of appetite, changes in taste, numbness and tingling, dry lips, mucosal lesions, difficulty swallowing, weight loss, constipation or diarrhea, constipation, tiredness and weakness or lack of energy, as well as changes in mood, anxiety, irritability, phobia and fear, uncertainty, difficulty concentrating, sleep disorders, among others. Since this is a complex and multidimensional phenomenon, contact as a grieving process and the meaning of death, the meaning of being in the hospital, and the pain and suffering present in the treatment itself, depending on the resources, were also presented as a characteristic of the experience of childhood cancer. offered for the management of the disease. It was possible to identify changes in the perception of self-image and shame related to it, as well as feelings of anger due to the interruption of contact with friends, the action of the denial of reality mechanism, and, not least, passive acceptance of therapeutic modalities, generating even more suffering in the child [31-33].
It is worth insisting and highlighting, as pointed out by Tutelman et al [34], that pain in children and adolescents related to neoplasms is characterized by the nature of the disease itself, such as being nociceptive, neuropathic, related to growth tumor, however, it is important to identify that this pain is also characterized by the diagnostic and/or management procedures used, especially when they are invasive procedures and also due to unwanted effects arising from the use of drugs.
It is also worth noting that non-pharmacological management resources can also have unwanted effects, however in the review carried out by LV et al. [35] points out that only 2 articles pointed to unwanted effects, such as bleeding and grade I hematomas present after the application of acupuncture or massage as a stimulus before more invasive procedures, which promoted fear in children. In addition to these records, no more serious unwanted effects were reported in other studies [36]
Thus, it is clear that childhood cancer pain is multifactorial, and, therefore, its control and management must also reflect these characteristics. The literature points out that the most effective management occurs when it involves interventions that consider its different dimensions and the language of pain itself [34,35].
It is the responsibility of specialized healthcare teams to adequately treat and manage pain regardless of etiology [33,34] points out that adequate control occurs in between 70% and 90% of cases, with the condition that specific and individualized therapies are applied to management, characterized by the combination of different methods, characterized by analgesic interventions and interventions non-pharmacological.
The characterization of pain can be described as acute due to its short duration or chronic occurrence, recurring over some time (for example, 3 months). One in five adults has chronic pain, leading to a huge economic cost of around $6 billion per year, greater than that for heart disease, cancer, HIV, and comorbidities. Chronic pain is also common in pediatric populations with average rates for several types of diseases, including cancer [37,38].
A Portuguese study, when evaluating the prevalence, pathologies and impact involved in pediatric chronic pain, observed particularities of this chronic pain, including the tendency for it to persist throughout life, with multiple recurrent episodes, resulting, in most cases, in numerous hospitalizations that interfered. in daily and school life in more than 50% of the children surveyed [39]. Some other studies point in the same direction, highlighting the impacts that diagnosis and treatment have on the lives of children and adolescents. It is estimated that around 80% of children with cancer, who are hospitalized, report painful experiences, and 50% of them evaluate this painful experience as intense. Of the children who remain in longer hospitalizations, 35% also report a painful experience [31-34,36]
Studies consider the possibility that pain is also related to longer hospitalization with a less stable clinical condition. For the authors, this idea was analyzed and is often linked to the effects caused by the temporality of the child's hospitalization, configuring, as well as internal (cancer - physical illness) and external (painful procedures) aggression for the child [40,41]
Given the reports, we observed that for these children/adolescents with cancer, although the painful location was presented more frequently, they also raised other contextual and affective dimensions. This fact leads us to reflect that pain cannot be thought of as a purely physical fragment, but a phenomenon extended to questions of existence, which reveal the past and present time, sometimes dissociating itself, sometimes integrating into the 'here-now of the cancer experience. As Angerami, et al. [42] describes, it is not enough to know where the pain is located, it is also necessary to be aware of the suffering of human beings based on their perception and expression.
Our results revealed that some children/adolescents perceived the painful effects more positively. However, the majority, when choosing Figure F, provide data on a negative response to pain, and such a response to pain carries the meaning of being minimized by the welcoming, comfortable, or safe environment, possibly favored by the family and the healthcare professional in general, which seeks better adaptation of the child/adolescent in the face of their physical and emotional vulnerability in the painful experience of cancer. Those represented by Figure I, equivalent to maximum pain, bring the need for greater physical, and psychological care and analgesic intervention, according to the meaning of the scale.
It is known that the unidimensional scale is considered a valid measurement instrument and reliable, fulfilling the objectives of quantifying and verifying the existence of pain, as well as analyzing whether the modulation is effective in different pain experiences [43]. However, it is worth noting that one-dimensional scales do not offer a broad perspective on the Algic experience. In this sense, multidimensional scales such as EMADOR [5] have the possibility of not only expanding the understanding of the pain experience but also offering data for the development of multidisciplinary management.
Regarding the data obtained with the application of EMADOR, the contingency of children's responses shows that, in different age groups, the details and logical elements expressed about the descriptors reveal that from five years of age, children are already able to attribute meaning to the pain phenomenon, in a categorical way, when verbalizations are referred to acute pain descriptors, with a high level of correlation with the concrete thought described by Piaget, et al. [44], thus demarcating the possibility of elaborating thought about pain as a function of their experiences, from the perspective of development in the life cycle.
In an older study from the 90s, which one of the objectives was to find out, in 41 hospitalized children (preschoolers), the words used to describe the experience of pain from the guiding question: "What is your pain like?". The study corroborates ours, as it revealed a tendency for participants to use concrete terms of an evaluative or indicative nature, resulting in varied concepts described by preschoolers, whose age range is 02-07 years old [45].
Unlike the findings of the study above, we can observe that some of the verbalizations about the pain by children under 7 years of age bring evidence of accurate and precise meanings with responses close to other older age groups, which suggests a non-cognitive immaturity about your stage of thinking and belief about the painful aspects.
We understand that this study fills an existing gap in the assessment of pediatric pain as described by Rossato, et al. [46]: “An existing gap in the assessment of the quality of children's pain remains due to the absence of adequate instruments at the level of the child’s cognitive development”.
A study carried out by Carvalho, et al. [47], demonstrates that pain management in hospitalized children has been ineffective. Even considering standardized measurement and evaluation models, institutions have not fully presented adequate evaluation and intervention. The authors point out that the interventions of greatest interest have a pharmacological focus and that the focus of management is explicitly related to conditions arising from surgery and orthopedics when compared to those from other specialties. On the other hand, non-pharmacological management measures are used in a deficient way and care with the evaluation process with testing and retesting after the intervention is also reduced in the daily practice of hospitals. This practice goes against what the literature on pain indicates as more effective management resulting from the interaction between management composed of pharmacological and non-pharmacological resources. Given this, it is necessary to affirm the need for multidisciplinary teams to enable management more comprehensively, with individualization, but with resources coming from different health professionals with different backgrounds and, based on this scenario, identify and recognize the needs for integration of approaches different stages of development of the child or adolescent for an adequate assessment and consequent development of an appropriate intervention and care plan. To this end, the authors point out the need for continued educational and professional training and training on the part of health institutions.
Considering that the pain experience has a subjective character [5,47], and this characteristic reveals the complexity that needs to be considered, mainly, to observe whether children, when in early stages of development, are or are not capable of transmitting accurate and reliable information [48].
Given these variables, it is worth reflecting on whether the conduct of health professionals continues to underreport pain, even when equipped with valid scales for use as a resource in the assessment process. Some studies indicate that professionals with biomedical training value behavioral and physiological aspects and ignore the use of verbal resources with the numerical verbal scale. Data from an American study indicate that of 178 participants evaluated, 48.2% verbalized pain classified as intense, but only 15% of the professionals who evaluated them recorded this data. This highlights the importance of training professionals but also introduces the need to use instruments that are characterized as self-report and assessments that fully explore the variables of the pain experience, including their meaning considering the phase of the life cycle in which the user of the service is found [47,49-52].
According to the data in Table 5, when characterizing chronic pain, children aged 5-7 years with cancer gave higher scores to the descriptors 'painful', 'terrifying', 'strong', 'excessive', and 'boring'. Of these, the quality of pain dimensions emerges with a majority for the sensitive dimension (painful, strong, and excessive) about the affective (terrifying) and cognitive (boring). According to Costa, et al. [53], the pain in most people with cancer is moderate in intensity and of a sensory (or sensitive) nature, which can impair the rhythm of daily activities.
Based on the attribution of chronic pain provided by children in this age group, we can also consider that, to recognize their pain, they tend to construct thoughts focused on the occurrence of sensations in their bodies. This is consistent with the literature on pain in pediatrics, which states that the child's thinking is absolute, with difficulty changing the belief about pain, as a physical dimension [54]. Still in this age group, the lowest scores were for the descriptors 'disastrous' (cognitive), 'devastating' (cognitive), and 'harmful' (cognitive) about 'spreading' (sensitive) and 'frightening' (affective), meaning that the cognitive nature of pain was presented with lower scores attributed by this age group. We understand that this type of response to pain may be related to the fact that children still have concrete thinking.
In the age group 8-11 years old, the descriptors with the highest scores were 'cursed' (affective), 'nasty' (affective), 'boring' (cognitive), 'strong' (sensitive), and 'unbearable' (cognitive); while those with the lowest attribution were ‘overwhelming’ (affective), ‘persistent’ (affective), ‘suffocating’ (affective), ‘depressing’ (affective) and ‘distressing’ (affective). Among the five most attributed descriptors there was an equivalent proportion for the dimension of affective pain (damn and unpleasant) and cognitive (boring and unbearable) and with a predominance of affective dimension descriptors with lower attribution scores.
It is known that at this stage, the child's egocentric thinking is elaborated towards logical and reversible thinking. Linguistic entities are more expanded and operational [44]. With the records above, we verified this transition in terms of the child's overcoming when distinguishing the internal and external, extrapolating from the more sensitive painful perception to another, in which he can use cognitive and affective qualitative terms and, however, the affective response to pain it does not reach the point of being persistent or depressing, suffocating and distressing.
Regarding the pain perception of adolescents aged 12-18, the results showed the descriptors 'boring' (cognitive), 'unpleasant' (affective), 'uncomfortable' (sensitive), 'uncomfortable' (affective) and 'nauseous'( affective) with higher scores. In this result, we found that, although the cognitive dimension had a higher score in the 'boring' descriptor (M=8.48), the affective dimensions were more significant (unpleasant, uncomfortable, and nauseating). In this sense, we can highlight adolescents' capacity for introspection and psychological understanding, as they can abstract pain with an affective quality associated with psychological suffering [44,54,55].
It is known that the affective dimension of pain may be related to the affectivity of the child/adolescent with cancer. When we refer to the context of the word affectivity, which encompasses a myriad of moods and a living organization of meanings and psychological contents such as sadness, love, passion, envy, and hopelessness, among others, we seek to characterize it, not just as a simple content that sensitizes, pleasantly or unpleasantly, the conduct of human beings – but as one that, certainly, houses within itself a list of meanings and contents of its own.
Because of this, we can assume that the participants who matched more scores to the affective algic dimension are accepting the expectations of dealing with their pain immersed in the complexity of the universe of symbolic meaning and attribution of subjective qualities. Such subjective qualities are intertwined with people, objects, and places of experience. Thus, we appropriate the fact that the psychological subject “returns” the result of his psychic action in an evaluative quality [56,57].
In the analysis by age group, the results regarding chronic characterization demonstrated heterogeneity in the responses attributed to pain. Thus, children aged between 05-07 years old highlighted the sensitive dimension, significantly representing concrete reasoning, those aged 08-11 years old highlighted the quality of pain in both the affective and cognitive dimensions, representing the transition from concrete reasoning and abstract and, the adolescents understood pain mediated by its affective character, representing the complementarity of the logical-formal abstraction, described by Piaget, et al. [44].
This scenario shows that, despite living with the disease, the development of these children/adolescents still leaves the mark of the process, that is, it flows over time. Furthermore, it demonstrates that it is not possible to read the objective experience of pain or perceive it as a universal conceptual entity since it is a personal experience, and it is through language that the specific qualities of each pain can be expressed verbally. painful sensation, which differs significantly from each other [5].
Furthermore, it is worth highlighting that pain is a total and integrated experience, which requires an interdisciplinary approach. The topic has been studied repeatedly by professionals and researchers who have direct contact with the control of physical symptoms, which probably guides what is considered relevant and what is considered unimportant and, therefore, neglected [58].
As a result of the above, we defend a position that recognizes that pain is often experienced through physical sensations, but it is worth highlighting that issues of biological and physiological nature are not always the central elements in the constitution and understanding of the phenomenon itself. Algic. Total pain [59] presents itself as an invaluable resource in the assessment of cancer pain, allowing the recognition of the factors that make up this phenomenon, namely: physical, environmental, emotional, social, and spiritual [60].
Conclusion
In short, when interacting with the results of the present study, we cannot remain unaware of the fact that each child/adolescent needs to be perceived integrally, as a developing person, with history, cognition, will, and affection. All of these attributes are resources that need to be considered for a more comprehensive assessment than just painful intensity, that is, the assessment of the total pain experience.
The cognitive dimension of pain can be observed as children/adolescents with cancer demonstrate, in their situational context, skills to observe, identify, perceive, memorize, compare, classify, conceptualize, learn, and draw conclusions from the painful experience.
With the application of 50 acute and chronic pain descriptors, it was possible to capture the most and least important descriptors, in addition to understanding, through the Multidimensional Pain Assessment Scale (EMADOR), an innovative instrument of significant importance for assessing pain. pain also in children and adolescents, due to the ease of application and validity, as the words (pain descriptors) could be understood and responded to by both children and adolescents, in a consistent manner. It is important to highlight that by using this scale it was possible to observe the evolution of thinking in the age groups studied, especially painful thinking, encompassed in sensory, cognitive, and affective complexity.
Climbing the paths proposed by pain and its universes means agreeing with the unknown, venturing into possible shortcuts in the flow of thought, perception, and consciousness laid bare in discourse, in the way it captures descriptors, how it represents and names pain, All of this is only possible through a dive into the interiority of the characters investigated, the child/adolescent with cancer in the systemic web of their family relationships.
We understand that pain is a natural phenomenon similar to the act of living and dying, essential. As such, the phenomenon is perceived by children and adolescents with cancer with similar contours to the perception brought by adults, since it intrinsically contains symbolic dimensions impregnated with values and meanings dependent on the personal, affective, sociocultural, and historical context. Therefore, it the important to know how to manage it from the perspective of the anthropologist, the dental surgeon, the nurse, the physiotherapist, the psychologist, the doctor, or better, through interdisciplinarity.
Carrying out this investigation allowed us to trigger some reflections on the importance of knowing the sensory, cognitive, and affective dimensions present in pediatric cancer pain, opening up possibilities for more adequate, humane, and ethical pain management in Brazilian public health, in which the sum of objective and subjective components involved in the experience of children, adolescents, and families with cancer and pain.
We understand that when considering the child/adolescent, their expressiveness and experience of pain and cancer, a whole condition submerged in the alternations focused on health/illness, language/perception, and multifaceted pain, implicated in the experience full of historicity, comes to light, of affection and singularity.
This study appears as a motivator for evaluations and measures in public health, research, and clinical areas, with the purpose of adequate pain management in the two very significant periods of the human life cycle: childhood and adolescence, involved by the link of family and care context, with the possibility of being palliative, in such a way as to allow the end of life with comfort, peace and dignity.
References
1. Ministério da Saúde Instituto Nacional de Câncer José Alencar Gomes da Silva Ministério da Saúde Instituto Nacional de Câncer. (2022). Available in: https://www.inca.gov.br/sites/ufu.sti.inca.local/files//media/document//estimativa-2023.pdf
2. Da Silva GF, De Assis MTB, Pinto NBF. Cuidados Paliativos Na Criança Com Câncer: O Papel Do Enfermeiro Na Assistência Do Cuidar. Brazilian J Develop. 2021; 7(5). https://doi.org/10.34117/bjdv7n5-655
3. Godino-Iáñez MJ, Martos-Cabrera MB, Suleiman-Martos N, Gómez-Urquiza JL, Vargas-Román K, et al. Play Therapy as an Intervention in Hospitalized Children: A Systematic Review. Healthcare. 8(3). https://doi.org/10.3390/healthcare8030239
4. Mota HVA, Silva MR da, Júnior CJ dos S. Intervenção à Criança Hospitalizada e Ludoterapia: Revisão Integrativa. 2019 Jul 19;4(2):1141–1151. Available from: https://doi.org/10.28998/rpss.v4i2.7358
5. Sousa FAEF, Pereira LV, Cardoso R, Hortense P. Multidimensional pain evaluation scale. 2010 Jul 19;18(1):03–10.
6. Perissinotti DMN, Sardá-Junior J. Psicologia e Dor: o que você deve saber. Editora dos Editores; 2019 Jul 19;1:208p.
7. Salvaro MS, Zanine MTB, Hoepers NJ, Silveira RLP. 2021 Jul 19;11(1):43–65.
8. Lippi EÂA da C. Avaliação e mensuração da dor crônica advinda do câncer. 2011 Oct 27;. Available from: https://www.teses.usp.br/teses/disponiveis/22/22132/tde-30112011-101701/en.php
9. Cardoso RPS, Faleiros Sousa FAE. The Idendification and validation of the Brazilian Chronic Pain Descriptors. 2009 Jul 19;10(2):85–93.
10. Faleiros Sousa FAE, Pereira LV, Hortense P. Avaliação e mensuração da percepção da dor. 2008 Jul 19.
11. Linhares MBM, Doca FNP, Martinez FE, Carlotti APP, Cassiano RGM, Pfeifer LI, Funayama CA, Rossi LRG, Finley GA. Pediatric pain: prevalence, assessment, and management in a teaching hospital. 2012 Jul 19;45(12):1287–1294.
12. Cordova Junior VA. Desenvolvimento e Validação de Aplicativo de Celular para Avaliação de Dor Infantil. Governo do Estado do Pará. Fundação Santa Casa de Misericórdia do Pará. Diretoria de Ensino, Pesquisa e Extensão, Programa de Pós Graduação em Gestão de Saúde na Amazônia. MESTRADO PROFISSIONAL Gestão e Serviços em Saúde. Avaible from:https://mestrado.santacasa.pa.gov.br/wp-content/uploads/2023/01/DESENVOLVIMENTO-E-VALIDACAO-DE-APLICATIVO-DE-CELULAR-PARA-AVALIACAO-DE-DOR-INFANTIL.pdf
13. Hastorf AH, Schneider DJ, Polefka J. Percepção da Pessoa. 1973 Jul 19;.
14. Stevens SS. Psychophysics: introduction to its perceptual, neural and social prospects. 1975 Jul 19.
15. Faleiros Sousa FAE, Da Silva JA. Mensurando dor. 2005 Jul 19;6(4):680–687.
16. McGrath P. Report of the Subcommittee on Assessment and Methodologic Issues in the Management of Pain in Childhood Cancer. 1990 Jul 19;86(5):814–817.
17. McGrath P. A new analogue scale for assessing children’s pain: an initial validation study. 1996 Jul 19;64:435–443.
18. McGrath PJ. Pain in Children: Nature, Assessment e Tratamento. 1990 Jul 19;:466f.
19. Souza Rodrigues FS, Polidori MM. Enfrentamento e Resiliência de Pacientes em Tratamento Quimioterápico e seus Familiares. Rev Bras Can. 2012 Jul 19;58(4):619–627.
20. Motta, A. (n.d.). Intervenção Psicológica Lúdica para o Enfrentamento da Hospitalização em Crianças com Câncer Recreational Psychological Intervention for Coping with Hospitalization in Children with Cancer. 26(3), 445–454. https://www.scielo.br/j/ptp/a/7cm39Rsx3KZ4Q7qTQBsDSpQ/?format=pdf
21. Instituto Nacional de Câncer José Alencar Gomes da Silva. Incidência, mortalidade e morbidade hospitalar por câncer em crianças, adolescentes e adultos jovens no Brasil: informações dos registros de câncer e do sistema de mortalidade [Internet]. Rio de Janeiro: INCA; 2016 [acesso 2020 abr 25]. Disponível em: https://www.inca. gov.br/sites/ufu.sti.inca.local/files//media/document// incidencia-mortalidade-morbidade-hospitalar-porcancer.pdf
22. Cavicchioli AC, Menossi MJ, Lima RAG de. Cáncer infantil: el itinerario diagnóstico. 2007 Jul 19;15:1025–1032.
23. Cestari MEW, Zago MMF. A prevenção do câncer e a promoção da saúde: um desafio para o Século XXI. 2005 Jul 19;58(2):218–221.
24. Barr RD, Ferrari A, Ries L, Whelan J, Bleyer WA. Cancer in Adolescents and Young Adults: A Narrative Review of the Current Status and a View of the Future. 2016 Jul 19;170(5):495–501.
25. Camargo B, de Oliveira Santos M, Rebelo MS, de Souza Reis R, Ferman S, Noronha CP, Pombo-de-Oliveira MS. Cancer incidence among children and adolescents in Brazil: First report of 14 population-based cancer registries. 2010 Jul 19;126(3):715–720.
26. Diniz AB, Regis CDA, Brito NP de, Conceição LS, Moreira LMA. Perfil epidemiológico do câncer infantil em população atendida por uma unidade de oncologia pediátrica em Salvador-Bahia. Revista de Ciências Médicas E Biológicas. 2005 Jul 19;4(2). https://doi.org/10.9771/cmbio.v4i2.4185
27. Cagnin ERG, ListonFerreira NM, Dupas G. 2003 Jul 19;16(4):18–30. Available from: https://acta-ape.org/article/vivenciando-o-cancer-sentimentos-e-emocoes-da-crianca/
28. Ljungman G. Pain in paediatric oncology: interviews with children, adolescents and their parents. 1999 Jul 19;88:623–30.
29. Pereira CIP, Nascimento IB, Da Cruz AS, Volc SM, Tormen TH. Impactos Psicossociais e na Qualidade de Vida do Tratamento Oncológico em Crianças e Adolescentes. Revista Brasileira De Cancerologia [Internet]. 2023 Aug 10;69(3).
30. Paiano LAG. . Experiência de sintomas no câncer infantojuvenil durante o tratamento quimioterápico : com a palavra, o adolescente e o familiar. Acervodigital.ufpr.br. https://acervodigital.ufpr.br/handle/1884/72222
31. Chokshi SK, Ladas EJ, Taromina K, McDaniel D, Rooney D, Jin Z, Hsu WC, Kelly KM. Predictors of acupuncture use among children and adolescents with cancer. Pediatric Blood & Cancer [Internet]. 2017 Feb 8;64(7):e26424. Available from: https://doi.org/10.1002/pbc.26424
32. Çelebioğlu A, Gürol A, Yildirim ZK, Büyükavci M. Effects of massage therapy on pain and anxiety arising from intrathecal therapy or bone marrow aspiration in children with cancer. International Journal of Nursing Practice. 2014; 21(6): 797–804. https://doi.org/10.1111/ijn.12298
33. Twycross A, Parker R, Williams A, Gibson F. Cancer-Related Pain and Pain Management. 2015 Jul 19;32(6):369–384.
34. Tutelman PR, Chambers CT, Stinson JN, Parker JA, Fernandez CV, et al. Pain in Children with Cancer. 2017 Jul 19;1. Available from: https://doi.org/10.1097/ajp.0000000000000531Ting-Ting Lv, Jian-Wei Lv, Wang, S.-Y.,
35. Jiang C, Gu YJ, Liu HR. Efficacy of electroacupuncture nerve stimulation therapy for interstitial cystitis/bladder pain syndrome. 2019 Jul 19;39(5):467–472.
36. Ahmed M, Modak S, Sequeira S. Acute Pain Relief After Mantram Meditation in Children With Neuroblastoma Undergoing Anti-GD2 Monoclonal Antibody Therapy. 2014 Jul 19;36(2):152–155.
37. King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, et al. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. 2011 Jul 19;152(12):2729–2738.
38. Moulin DE, Clark AJ, Speechley M, Morley-Forster PK. Chronic Pain in Canada - Prevalence, Treatment, Impact and the Role of Opioid Analgesia. 2002 Jul 19;7(4):179–184.
39. Gonçalves ALVR. Dor crónica pediátrica em Portugal Caracterização da situação. 2008. Dissertação (Mestrado em ciências da dor) Universidade de Lisboa, Faculdade de Medicina de Lisboa, Lisboa, 2008
40. Souza RLA de, Mutti CF, Santos RP dos, Oliveira DC de, Okido ACC, Jantsch LB, Neves ET. Hospitalization perceived by children and adolescents undergoing cancer treatment. 2021 Jul 19;42. Available from: https://doi.org/10.1590/1983-1447.2021.20200122
41. Prates EJS, Prates MLS, Bueno TR, Shimoda S, Souza CBL. Escalas de dor em pacientes oncológicos pediátricos: Uma revisão de literatura. 2018 Jul 19;5(2). Available from: https://doi.org/10.18406/2359-1269v5n2201877
42. Angerami VA. Psicossomática e a Psicologia da Dor: 2ª edição revista e ampliada. Cengage Learning Brasil; 2016 Jul 19.
43. Freitas CC. Avaliação da dor com o uso das escalas unidimensionais. Rev Dor . 2009 Jul 19;10(1):56–62.
44. Piaget J, Inhelder B. Grupo Editorial REcord; 2021 Jul 19.
45. Rossato LM, Angelo M. Utilizando instrumentos para avaliação da percepção de dor em pré-escolares face a procedimento doloroso. 1999 Jul 19;33(3):236–249.
46. Rossato LM, Magaldi FM. Multidimensional tools: application of pain quality cards in children. 2006 Jul 19;14(5):702–707.
47. Carvalho JA, Souza DM de, Domingues F, Amatuzzi E, Pinto MCM, Rossato LM. Pain management in hospitalized children: A cross-sectional study. 2022 Jul 19;56. Available from: https://doi.org/10.1590/1980-220x-reeusp-2022-0008en
48. BARROS L. Psicologia Pediátrica: perspectiva desenvolvimentista. 2003 Jul 19.
49. Skog N, Mesic Mårtensson M, Dykes A, Vejzovic V. Pain assessment from Swedish nurses’ perspective. 2020 Jul 19;26(3).
50. Peng N, Lao AH, Chen C, Lee M, Chiang L, Chang Y, Liu H. Knowledge and attitudes of pediatric clinicians regarding pediatric pain management. 2020 Jul 19;25(4). Available from: https://doi.org/10.1111/jspn.12302
51. Zisk-Rony RY, Lev J, Haviv H. Nurses’ Report of In-hospital Pediatric Pain Assessment: Examining Challenges and Perspectives. 2015 Jul 19;16(2):112–120.
52. Thrane SE, Wanless S, Cohen SM, Danford CA. The assessment and non-pharmacologic treatment of procedural pain from infancy to school age through a development lens: A synthesis of evidence with recommendations. 2016 Jul 19;31(1):E23–E32.
53. Costa AIS, Chaves MD. Dor em pacientes oncológicos sob tratamento quimioterápico. 2012 Jul 19;13(1):45–49.
54. Okada M, Teixeira MJ, Myagi KT. Tratamento da dor em pediatria. 2001 Jul 19;80(1):157–169.
55. Chagas V, Rodrigues N, Maria M, Bezerra D, Alberto C, Bushatsky M. Percepção do Adolescente frente à sua Condição de Adoecimento Oncológico. 2021 Jul 19;67(4). Available from: https://doi.org/10.32635/2176-9745.rbc.2021v67n4.1672
56. Sant'Anna PA. Arquétipo, individuação e intersubjetividade: a dimensão psicossocial do sofrimento humano. 2019 Jul 19;14(4):1–12. http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1809-89082019000400005&lng=pt&tlng=pt.
57. PINTO FEMO. Os (des)afetos da inteligência: o possível diálogo entre cognição e afetividade. 2005 Jul 19;13(1):7–12
58. Rimet Alves de Almeida H, Freitas de Melo C. Orthotanasia and dignified death in cancer patients: The perception of health professionals. 2019 Jul 19;:143–160. Available from: https://pesquisa.bvsalud.org/portal/resource/pt/ibc-184804
59. CLARK D. New York, Ny: Oxford University Press; 2018 Jul 19;.
60. Gomes A, Melo C de F. DOR TOTAL EM PACIENTES ONCOLÓGICOS: UMA REVISÃO INTEGRATIVA DA LITERATURA. 2023 Jul 19;28:e53629.https://doi.org/10.4025/psicolestud.v28i0.53629
Received: March 25, 2024;
Accepted: April 22, 2024;
Published: April 23, 2024.
To cite this article : de Oliveira Moura Siqueira HB, Vilarindo AB, Falconi Gomez RR, Saltareli S, Raminelli da Silva TDC, Faleiros Sousa FAE. The Perception of Pain in the Experience of Childhood Cancer. British Journal of Cancer Research. 2024; 7(1): 670- 680. doi: 10.31488/bjcr.192.
© The Author(s) 2024. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/).
