Research article / Open Access
DOI: 10.31488/bjcr.168
The Prevalence of Psychosocial Distress among Cancer Patients: A Single Institution Experience at the State of Qatar
Azza Hassan1,2, Azar Naveen Saleem1, Saad Jobran Eziada1, Abdelsadiq Bashir1, Amna Gameil1, Hind Elmalik1, Ayman Allam1
1. National Center for Cancer Care and Research, HMC, Doha, Qatar
2. Cancer Management & Research, Medical Research Institute, Alexandria University, Egypt
*Corresponding author: Azza Adel Hassan, National Center for Cancer Care and Research, HMC, Doha, Qatar; Cancer Management & Research, Medical Research Institute, Alexandria University, Egypt
Abstract
Introduction: The prevalence of psychosocial distress is up to 45% among cancer patients. It is crucial to identify and treat distress in order to improve the quality of life, satisfaction and assure adherence to cancer therapy and ultimately increase survival rates. The aim of the study is not only to report on the prevalence of distress among cancer patients but to also analyze the variable causes of distress as well as to study the effect of the disease stage using the Distress Thermometer. Methods: We studied distress among 3 groups, each consisting of 100 patients: those initially diagnosed, patients undergoing treatment, and patients who were referred to the palliative team. Different variables such as time of screening, sex, age, nationality, and tumor type were analyzed. Results: There was an overall distress incidence of 62% (level ≥ 4) and out of that 17% of the patients had severe distress (level >7). Similarly, there was 75% of distress among patients who were referred to palliative care, compared to 56% of patients at initial diagnosis and 54% for those undergoing cancer treatments. In addition, women (69%) had more distress than men (53%). Expatriates had higher levels of distress, compared to Qataris (64.3% versus 51%). Breast (69%) and lung (70%) cancer patients had the highest level of distress. Physical causes of distress were the most common (80%), followed by emotional causes (69%). Conclusion: There is a substantially higher overall incidence of distress among cancer patients in Qatar compared to that reported internationally. Patients referred to palliative care, those with breast and lung cancers had the highest level of distress. Distress screening should be considered as an essential component of the assessment of patients at diagnosis, repeated at regular intervals, especially at the time of disease progression. Screening alone is not enough; the different causes of distress should be identified and addressed by the appropriate interventions.
Keywords: Screening, psychosocial distress, cancer
Introduction
Psychosocial Distress is defined as an unpleasant emotional, psychological, social, or spiritual experience that interferes with the ability to cope with cancer and/or its treatment. It extends along a continuum from the normal feeling of vulnerability, sadness to real disabling problems such as true depression, anxiety, panic, and spiritual crisis [1,2]. This distress can be present in form of physical symptoms such as fatigue, pain, nausea and vomiting, sleep disorder, loss of weight, all of which don’t respond to traditional treatment [3]. According to international studies, psychosocial distress was found to be a common health problem among cancer patients ranging from 15% at early cancer diagnosis to around 60% upon referral to palliative care [4]. Failure to identify and treat anxiety and depression increases the risk of distress. The following factors have been identified as the causes for the increased incidence of distress such as recurrent, advanced, or progressive disease, younger age, female gender, lack of social support and history of previous psychiatric illness [5,6]. The National Comprehensive Cancer Network (NCCN) states that “Distress extends along a continuum, ranging from common normal feelings of vulnerability, sadness, and fears to problems that can become disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis" [7]. Being distressed isn’t a pleasant experience; It may affect how well the patient or even the caregiver’s function. Distress may also interfere with health decisions or actions. Distress can occur at any point in time during the patient’s cancer journey. Identifying and treating distress is crucial and it helps the cancer patients to stay more compliant with the treatment. Like all the cancer centers in the world the National Center for Cancer Care and Research (NCCCR), Hamad Medical Corporation (HMC), Qatar also has distress as a major challenge among cancer patients. NCCCR currently does not have the practice of screening distress among cancer patients despite the international recommendations for screening and to consider distress screening as a sixth vital signs [8-10]. We believe that identifying and implementing a system for screening distress shall relieve suffering, improve patient’s outcome, encourage the delivery of support services on an individual basis and enrich the quality of life.
Several tools have been identified and used in the screening of psychosocial distress among cancer patients, the most used tools are Depression-Anxiety Hospital Scale (DAHS), The Distress Thermometer (DT), and the Distress Assessment and Response Tool (DART).
DT is by far the most used, simplest, and mostly validated tool adopted in many centers. It is composed of two parts, a scale from zero to 10 to determine the severity of distress and a second part related to patients life in more details (Family, practical, emotional, physical problems as well as spiritual and religious concerns) [7,8]. This tool has proved to be effective both in hospital and in community settings.
Aim
The goal of the study is to assess the prevalence of psychosocial distress among cancer patients at National Center for Cancer Care and Research (NCCCR), Qatar at different stages of their disease as well as to identify the most common causes for this distress using the DT as a tool. We also aim to compare the intensity of distress among the variable demographic entities.
Methods
A total of 300 patients were studied from January 2015 up to December 2015. We categorized the patients into three groups, each consisting of 100 patients. The three groups were categorized based on (a) those initially diagnosed with cancer (group 1), b) patients undergoing cancer treatment (group2), and (c) patients with progressive disease who were referred to palliative care (group3). Different variables such as time of screening, sex, age, nationality, and tumor type were analyzed. Cancer patients aged 16 years and above were enrolled in the study. Participants were identified through existing records held at HMC and NCCCR. Participants were asked to take part in the study by the clinicians. In-patients, outpatients, daycare unit patients and radiotherapy patients were included in the study. Data was collected at HMC and NCCCR by using the DT tool over a period enough to collect samples of 300 cases. For the inpatients, the data was collected in the ward at their convenience. Similarly, for patients receiving chemotherapy or radiotherapy, they were given the DT tool to be completed at the daycare unit or in the radiotherapy department either before or after treatment session according to their preferences while outpatient participants were asked to take part following their regular visits at the clinic. The physicians were present during the filling of the survey and assisted with the queries the participant had. The filling of the DT took 5-10 minutes on average. The DT tool records the number (0-10) that best describe how much distress the patient has been experiencing in the past week including the day of assessment (e.g.0 has no distress and 10 have extreme distress). Responses are made on a 10-point scale. Low scores ranging from 0-3 meant mild distress not requiring any intervention, scores from 4-7 meant moderate degree of distress that can affect patient’s life; while those who scored from 8-10 had a high level of distress that can significantly affect their life and compliance with cancer treatment. The primary outcome measure was to assess the severity of distress according to the score of DTs at different stages of the disease trajectory. Secondary measures included the description of the detected problems from the lists of the various factors contributing to distress.
Analysis
Descriptive statistics were used to summarize the collected data on the severity of distress at different stages of the patient’s diseases. Chi-square test was applied to examine an association between severity of distress with demographic and different factors related to problems like practical, emotional, and physical.
All P values presented were two-tailed, and P values were considered as statistically significant if ≤ 0.05. All Statistical analyses were done using statistical packages SPSS 22.0 (SPSS Inc. Chicago, IL) and Epi-info (Center for Disease Control and Prevention, Atlanta, GA) software.
Results
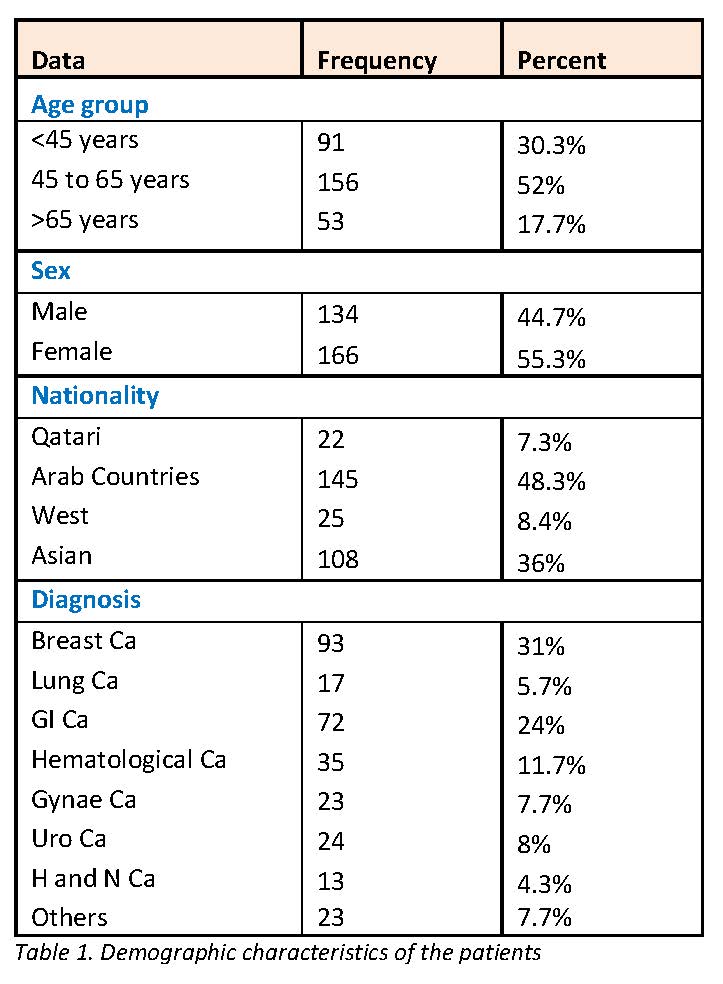
We screened 300 adult cancer patients. The patients were categorized into three groups, 100 patients at the time of initial diagnosis with cancer (group 1), 100 patients undergoing cancer treatment (group 2), and the last group included patients with progressive disease who were referred to palliative care (group3). Fifty five percent of patients were females compared to forty five percent males. The majority (52%) of the patients were in the middle age group between (45-65) years of age followed by 30% < 45-year-old and lastly 17% aged >65 years.
Out of 300 patients, only 7.3 % were Qatari Nationals while 48.3% from other Arab countries and remaining 44.3% belong to Non-Arab Asian countries and the West. The most common type of cancer among the studied patients were breast cancer (31%) followed by G.I cancer (24 %) and hematological malignancies (11.7%) (Table1).
Table 1:Demographic characteristics of the patients
There was an overall distress incidence of 62% (95% Confidence interval 56.4, 67.3) (distress score level ≥ 4), out of that 17% of patients had severe distress (distress score level > 7) (Graph 1). The mean distress score was 4.5 ± 2.78 (range 0-10). There was a significantly higher level of distress observed among patients who were referred to palliative care (75%) compared to (54%) those who were at their initial diagnosis and (57%) of patients undergoing treatment; (P=0.004) (Graph 2). The incidence of distress was significantly higher among women (69.3%) compared to men which were (53%), (P=0.004) (Graph 3). Age had no impact on the level of distress (Table 2). Expatriates had higher levels of distress, compared to Qatari nationals (64.3% versus 59%), however, their difference was statistically insignificant (P=0.28). Breast (69%) and lung (70%) cancer patients had a higher incidence of distress. In our study we found that the level of distress is more significant among patients with practical, emotional, physical, and family problems. Level of distress was statistically higher among patients who have practical problems compared to those who didn't have practical problems (69.5% s 46.4%, P=0.001). However, when we look at the components of the practical, emotional, physical and family problems individually the difference in level of distress noted was statistically insignificant (Table 2). Our study also showed that the spiritual problems had no effect on the level of distress among our patients (p=0.55).
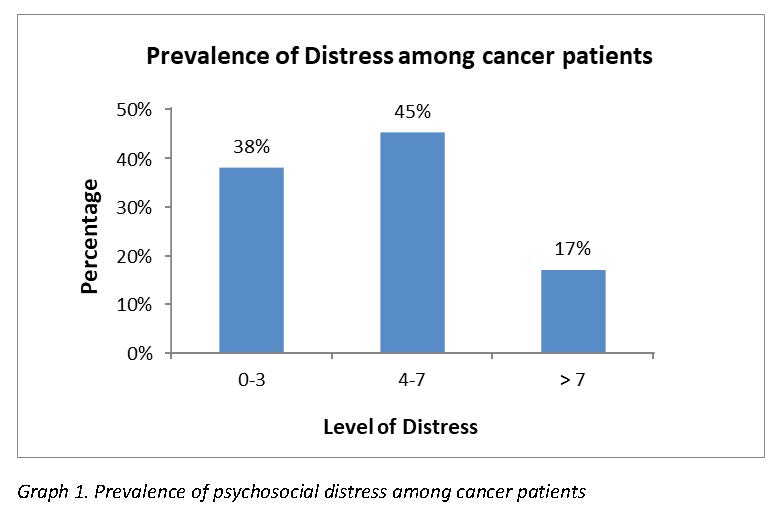
Graph 1:Prevalence of psychosocial distress among cancer patients
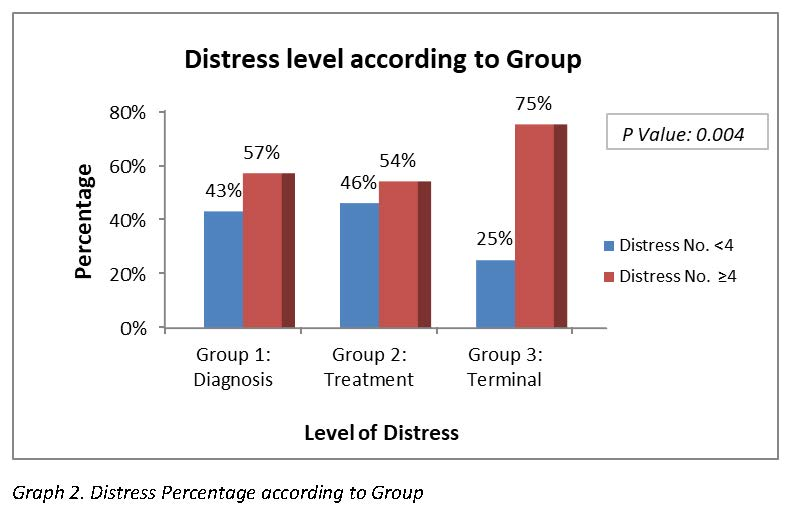
Graph 2:Distress Percentage according to Group
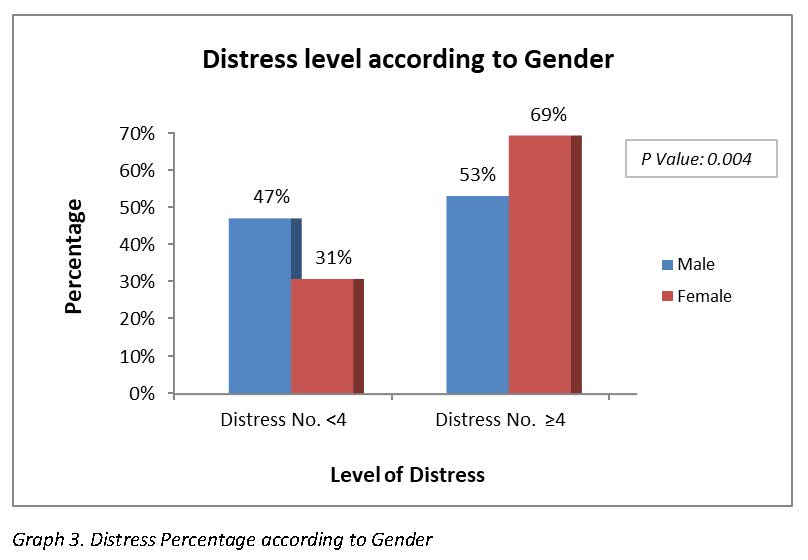
Graph 3:Distress Percentage according to Gender
Table 2:Comparison of Demographic and clinical characteristics between patients with and without psychosocial distress
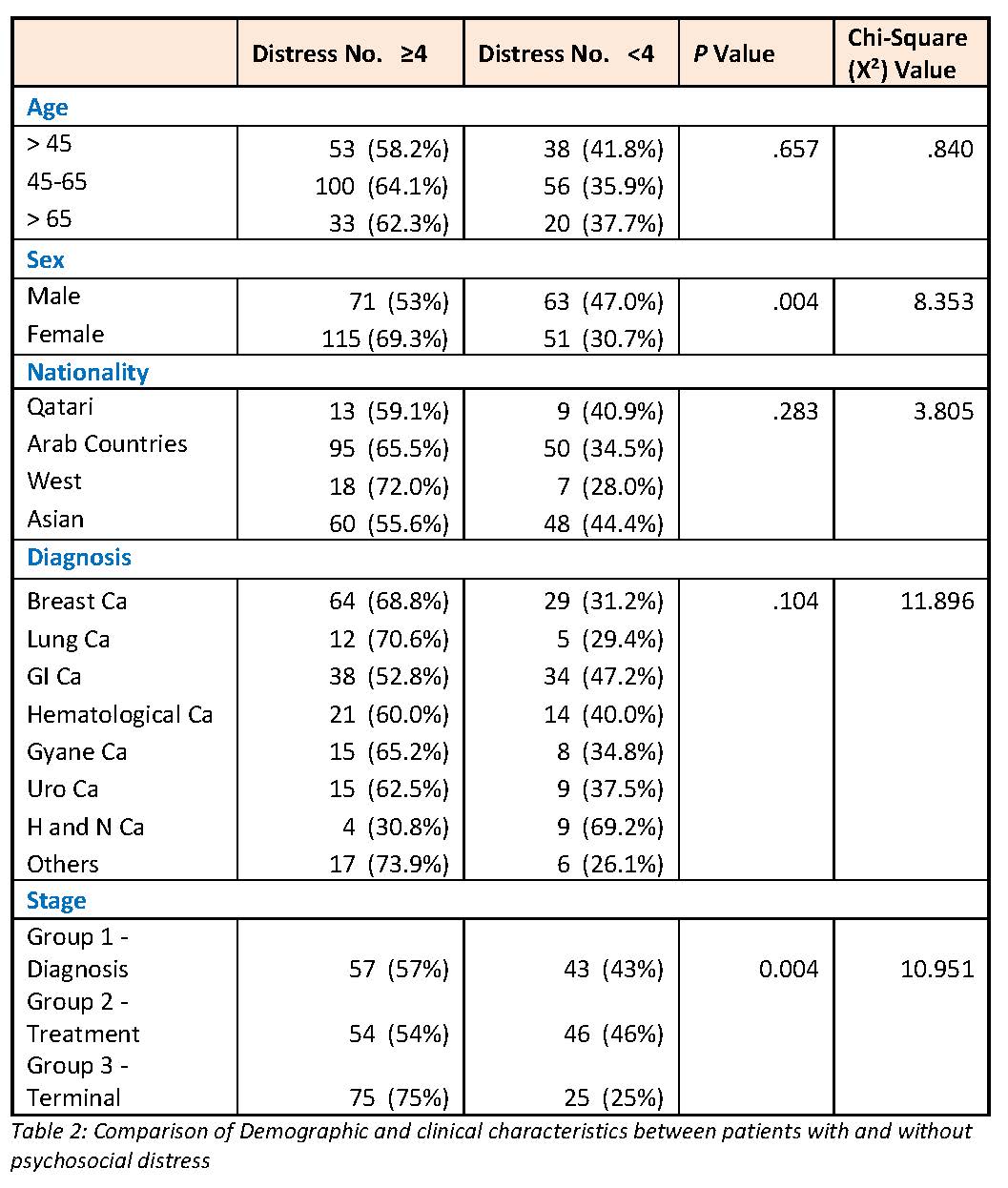
* Signifies that there is a problem in any one of the components under the main problems namely Practical, emotional, physical, or family problems
Discussion
In the present study, the overall incidence of distress (≥ score of 4) was 62% which is much higher than that reported internationally (ranging from 25% to 45%) [13]. This higher incidence has also been noted in a study from Saudi Arabia [12] where the incidence of moderate to severe distress was 57.3%. This can be attributed to the fact that most of the population in both countries is expatriates who live alone and lack of psychosocial support.
Results from this study showed significantly higher incidence of distress among women compared to men (69% versus 53%, p=0.004). This finding could be due to the fact of a higher incidence of distress in breast cancer cases (69%) which is more common among females. It is also known that female cancer patients are more emotionally labile and depressed compared to male cancer patients. This finding was also seen in a study performed at the Edinburgh Cancer Center which showed a higher incidence of distress among females compared to males (25% versus 17% respectively) [14]. The level of distress is affected by cancer type Carlson et al reported in 2019 a higher level of distress among pancreatic and lung cancer cases is more than 4500 cases treated in 55 North American Cancer Centers [11]. This finding was also confirmed by another study which reported higher incidence of distress in patients with lung, pancreatic and head and neck cancers [15]. In a large cohort of patients with cancer diagnosis, Linden et al reported a higher level of anxiety and distress in patients with Lung, gynecological or hematological cancer [16].
In our present study, higher level of distress (≥ 4) were found in lung cancer (71%), Breast cancer (69%), gynecological (65%) and hematological (60%) malignancies. This is in accordance with the previously reported literature, except that we had a higher incidence of significant distress in breast cancer cases. This finding could be attributed to the higher prevalence of breast cancer in our cohort of patients (31% of cases).
In this study, the incidence of distress was significantly higher (75%) among the group of patients with progressive advanced disease who were referred to Palliative care compared to those at initial diagnosis or during cancer therapy (54% and 57% respectively). This finding is in complete agreement with the reported incidence in the literature. A Korean study in 2017 reported a significantly higher level of psychosocial distress in advanced stages of gastric cancer compared to earlier stages [17]. The same finding was also reported among patients with the diagnosis of Sarcoma in a Canadian trial in 2019 [18] where patients with unresectable or metastatic disease had significantly higher psychosocial distress compared to patients with early operable disease.
An earlier study in 2008 [19] reported a significantly higher level of distress for patients treated in in Palliative care compared to patients recruited from hospitals and outpatient clinics (p <0.001). Also, a German study on bladder cancer revealed a significantly higher distress level and expressed need for psychosocial support in patients with progressive disease compared to those at first diagnosis [20].
To the best of our knowledge, this is the first study in the Middle East to compare the incidence of distress at 3 different stages of the disease (at initial presentation, during therapy and upon referral to palliative care). This means that assessment of psychosocial distress should be performed at regular intervals during the patient trajectory with cancer.
We also found that the incidence of distress was slightly higher among expatriates (64%) compared to Qatari nationals (59%). This difference could be attributed to the lack of adequate psychosocial and family support among expatriates, who are usually alone.
In our study we found that the level of distress was more significant among patients who had practical, emotional, physical, and family problems. The level of distress was statistically more significant among patients who had practical problems compared to those who didn't have practical problems (69.5% vs 46.4%, P=0.001).However, when we look at the components of the practical, emotional, physical and family problems individually the difference in level of distress noted disappears. Our study also showed that the spiritual problems had no effect on the level of distress among our patients. (p=0.55). A similar result from Saudi Arabia [12] showed that the level of distress is significantly higher among the patients with practical, emotional, physical and family problems except the spiritual problem which is in accordance with our study. The individual components analyzed in our study provides vital information to identify the possible causes of distress in the State of Qatar and help us in adapting new effective interventions to minimize distress among our cancer patients.
Limitations
The study did not intend to assess the role of different strategies to minimize the level of distress. However, we shall address this issue with our upcoming research. Few potential predictors related to distress example: employment, marital status, educational status, psychiatric evaluation has not been captured in the current study. The study being the first attempt to assess the psychosocial prevalence among the cancer patients in the State of Qatar, It haven’t assessed the psychosocial distress level among the cancer patients with different stages of the disease (For group 1 and 2)
Conclusion
The present study clearly demonstrates a higher percentage of distress in Qatar compared to that reported internationally. Patients referred to palliative care, female patients, those with breast and lung cancers had the highest level of distress. The early identification of distress and its severity among cancer patients serves as a guide to us to address this problem. Patients scoring more than 4 can be identified earlier and referred to appropriate professionals according to their problems for further assistance. This emphasizes the fact that distress screening helps in early identification of distress and its severity among cancer patients. The availability of the multi-disciplinary team such as psychotherapy, psychiatry, social services, spiritual services, and counseling services along with the palliative care can identify, treat, and follow up distress among the patients throughout their cancer journey. This is the first study at NCCCR to assess cancer patients from the psychosocial aspect and manage them accordingly. Also, the results from the study may have positive consequences on screening to manage them accordingly in the future studies. The easy practical adaptability of this simple distress tool also helps in implementing this tool in our daily practice. We hope that the results of this study will reflect on the initial assessment of our cancer patients and consider distress screening as the 6th vital sign. It also helps us to integrate psychosocial care into our routine cancer treatment pathway to enhance patient care.
References
1. Vitek L, Rosenzweig MQ, Stollings S. Distress in patients with cancer: definition, assessment and suggested interventions. Clin J Oncol Nurs. 2007; 11(13): 413-418
2. Velikova G. Patient benefits from psychosocial care: Screening for distress and models of care. J Clin Oncol. 2010;28: 4871-4873
3. Jacobsen PB, Donovan KA, Vadaparampil ST, et al: Systematic revies and meta-analysis of psychological and activity-based interventions for cancer-related fatigue. Health Psychol. 2007;26: 660-667
4. The International Endorsement of US Distress Screening and Psychosocial Guidelines in Oncology: A model for Dissemination. Mark Lazenby at the Journal of the National Comprehensive Cancer Network. 2014; 12 (2):221-227.
5. Okamura H, Watanabe T, Narabayashi M. et al: Psychological distress following first recurrence of disease in patients with breast cancer: Prevalence and risk factors. Breast Cancer Res Treatment. 2000; 61:131-137.
6. Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005; 103: 1949-1502
7. The National Comprehensive Cancer Network. Distress management clinical practice guidelines in Oncology. Version.3. 2015. Available at www.nccn.org
8. NCCN Distress Thermometer for patients (NCCN 2010), Clinical Practice Guidelines in Oncology. Available at www.nccn.org
9. Canadian Association of Psychosocial Oncology Conference: Statement of Endorsement; Screening for Distress as the 6th vital sign. April 2009, Vancouver, Critish Colombia, Canada
10. Union for International Cancer Control. Distress the 6th vital sign in cancer care2010.
11.Carlson LE, Zelinski EL, Toivonen KI, et al. Prevalence of psychosocial distress in cancer patients across 55 North American cancer centers. J Psychosoc Oncol. 2019;37(1):5-21.
a. Zuhoor AL-Gaithy, Atlal Abusanad, Fatima Arab. Psychological Distress among Cancer Patients from Saudi Arabia. Int J Art & Humanity Sci. 2017; 4: 16-24.
12. Mertz BG, Bistrup PE, Johansen C, et al. Psychological distress among women with newly diagnosed breast cancer. Eur J Oncol Nur. 2012; 16: 439- 443.
13. Strong V, Waters R, Hibberd C, Rush R, Cargill A, Storey D, Walker J, Wall L, Fallon M, Sharpe M. Emotional distress in cancer patients: the Edinburgh Cancer Centre symptom study. Br J Cancer. 2007 Mar 26;96(6):868-74.
14. Carlson LE, et al. “High levels of untreated distress and fatigue in cancer patients.” Brit J Canc. 2004; 90: 2297-304.
Received: August 10, 2021;
Accepted: August 24, 2021;
Published: August 27, 2021.
To cite this article : Hassan A, Saleem AN, Eziada SJ, et al. The Prevalence of Psychosocial Distress among Cancer Patients: A Single Institution Experience at the State of Qatar. British Journal of Cancer Research. 2021; 4:2.
©2021 Hassan A, et al. .
